Abstract
The rapidly developing field of cell therapy uses live cells to treat a wide range of illnesses, including as cancer, autoimmune diseases, and degenerative problems. The important roles that stem cell therapy, CAR-T cell therapy, and immune cell therapy play in neurological, regenerative, and oncological treatments are examined in this article. The precision of these therapies has been improved by innovations such as induced pluripotent stem cells (iPSCs) and CRISPR gene editing. But issues like exorbitant prices, worries about safety, and ethical discussions—particularly in relation to embryonic stem cells—remain. With more research done, cell therapy has the potential to transform medicine by offering individualized and focused therapies.
Introduction
Cell therapy, which replaces or repairs damaged tissues and organs with living cells, is becoming more common as a treatment option for a variety of disorders as medical advances. It is becoming increasingly popular, particularly in cancer immunotherapy and regenerative medicine. Significant progress has been achieved with CAR-T cell therapy, which alters a patient’s immune system to target and eliminate cancer cells. This method has been successful in treating lymphoma and leukemia. Furthermore, stem cell therapy has great potential for restoring damaged tissues in situations like heart disease, neurological problems, and spinal cord injuries.
Recent developments in gene-editing technologies, such as CRISPR, are expanding the potential applications of cell therapy by enabling more precise modifications to improve treatment effects. Nonetheless, there are still hurdles to overcome, such as financial limits, legal impediments, and moral quandaries—particularly over the use of embryonic stem cells in certain medical therapies. Despite these challenges, cell therapy has the potential to revolutionize medicine by providing more individualized and efficient treatment choices as research progresses.
Section 1: What is Cell Therapy?
The use of living cells for medicinal purposes, known as cell therapy, aims to treat or cure diseases by replacing, mending, or enhancing the biological function of damaged organs or tissues. These therapies target diseases by changing the immune system, encouraging healing, or regenerating tissue, either with the help of the body’s own cells or the introduction of new ones. The process typically comprises removing cells from the patient or a donor, processing the cells in a laboratory, and then returning the cells to the patient.
One of the most widely used forms of cell therapy is stem cell therapy. Mesenchymal and hematopoietic stem cells in particular have the extraordinary capacity to differentiate into specialized cell types and repair injured tissues. This technique has shown potential in treating disorders such as leukemia, spinal cord injuries, and cardiac difficulties.
CAR-T cell therapy, which alters T-cells, an immune cell subtype, to recognize and eradicate cancer cells, is another important breakthrough in treatment. This therapy has shown remarkable results, especially in the treatment of leukemia and lymphoma, two blood cancers. Furthermore, research is being done to see whether other immune cell therapies, including as dendritic and natural killer (NK) cell therapies, can boost the body’s defenses against cancer and infections.
Cell therapy is not limited to use in oncology and regenerative medicine. Cell therapies help reduce inflammation and prevent tissue damage by altering the immune system in autoimmune diseases. All things considered, the science of cell therapy is one that is developing quickly, has a vast array of possible applications, and has the power to dramatically change how many challenging diseases are treated.
Section 2: Types of Cell Therapies
Cell treatments encompass a broad spectrum of methodologies that leverage the diversity of cell types to specifically target specific diseases. While there are many distinct types of cell therapies, the most well-known and frequently utilized ones are immunological, CAR-T, and stem cell therapies; each has unique advantages for treating certain medical conditions.
Stem cell treatment, which utilizes stem cells’ ability to differentiate into other cell types, is arguably the most versatile. The two most typically used types are mesenchymal stem cells (MSCs) and hematopoietic stem cells (HSCs). Because MSCs can repair muscle, bone, and cartilage, they are crucial for treating conditions like osteoarthritis and cardiovascular illnesses. On the other hand, HSCs are mostly used in bone marrow transplants to cure cancers connected to blood, like leukemia and lymphoma.
CAR-T Cell Therapy is an advanced immunotherapy wherein T-cells are genetically modified to specifically target cancer cells. It is possible to modify the patient’s own T-cells such that they express chimeric antigen receptors (CARs), which improves their capacity to recognize and destroy cancer cells. This medication has shown remarkable outcomes in the treatment of B-cell malignancies, particularly acute lymphoblastic leukemia.
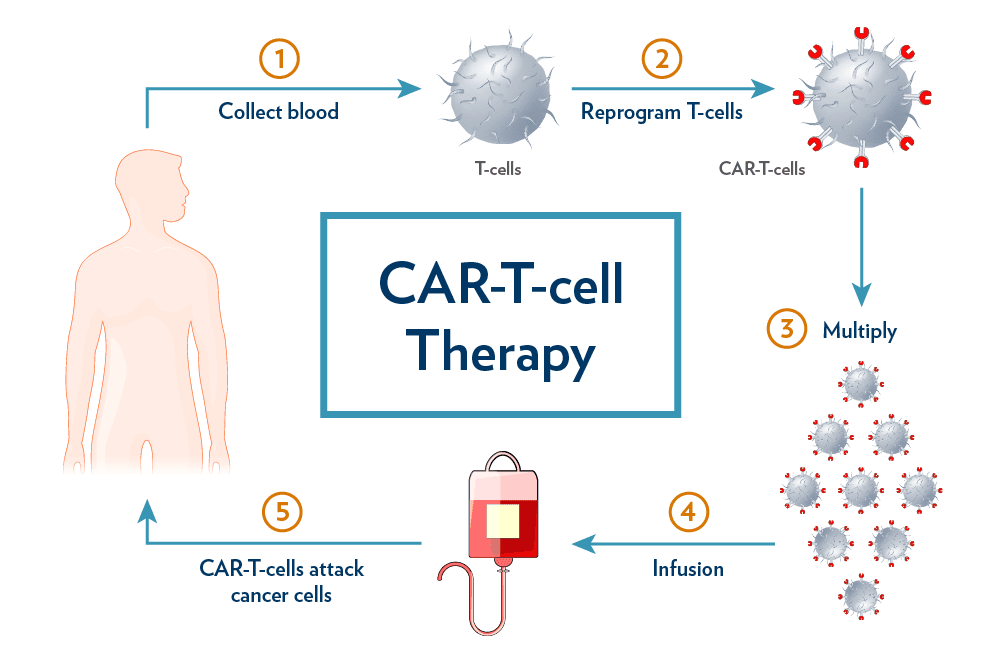
Fig.1 CAR-T Cell Therapy Process
Boosting the immune system’s natural ability to combat disease is the aim of immune cell therapies, including dendritic and natural killer (NK) cell therapy. Dendritic cell therapy presents antigens to T cells in order to stimulate an immune response, whereas NK cell therapy targets tumor cells with the intrinsic cytotoxicity of NK cells.
Taken together, these diverse cell therapy types show the great potential and range of applications for treating a wide range of diseases, from cancer to degenerative disorders.
Section 3: Key Applications of Cell Therapy
In several medical professions, cell therapy has fundamentally altered the way diseases that were previously difficult to cure are managed. Because of its ability to target cancer cells, alter immune responses, and repair tissues, it is a valuable tool in modern medicine.
Oncology is likely the field where cell therapy is used in its most advanced form. By genetically modifying T cells to specifically target cancer cells, CAR-T cell therapy has shown extraordinary efficiency in treating some blood cancers, including acute lymphoblastic leukemia and B-cell lymphomas. Natural killer (NK) and dendritic cell therapies are also being developed to target solid tumors in an effort to broaden the application of cell-based medications in cancer therapy.
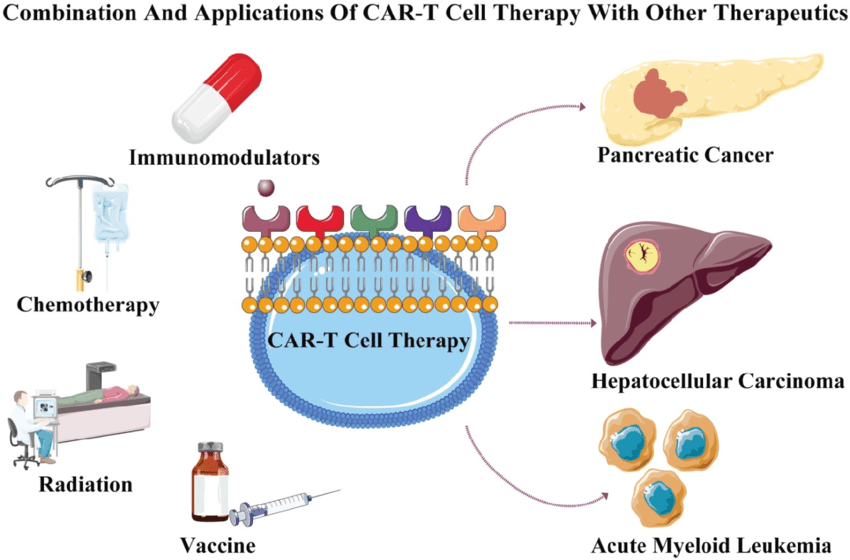
Fig.2 Combination and applications of CAR-T cell therapy with other therapeutics
The use of stem cells in regenerative medicine is very important. Mesenchymal stem cells have the ability to regenerate damaged heart muscle, bone, and cartilage (MSCs). This is particularly useful in the treatment of conditions like osteoarthritis, myocardial infarction, and spinal cord injuries. Furthermore, studies are being conducted on the utilization of stem cells to regenerate liver and pancreatic tissues, which could result in the creation of medications to treat liver and diabetes.
In autoimmune illnesses, cell therapy is utilized to alter the immune system. Treatments targeting regulatory T-cells (Tregs) are useful for multiple sclerosis and rheumatoid arthritis because they work by reducing the immune response. These therapies can prevent tissue damage and reduce chronic inflammation.
Cell therapy is also making progress in the treatment of neurological illnesses. Stem cell-based therapies have shown promise in the management of neurodegenerative conditions like Parkinson’s, Alzheimer’s, and spinal cord injuries. These therapies aim to restore damaged neurons and encourage nerve regeneration.
Section 4: Advances in Cell Therapy Research
Recent developments in biotechnology and genetic engineering have greatly expanded the applications of cell therapy. The use of CRISPR-Cas9 gene editing, which enables precise cell alterations to improve therapeutic potential, is one of the most noteworthy innovations. For example, CRISPR is being utilized in CAR-T cell therapy to better modify T-cells so they can target and kill cancer cells more efficiently. Furthermore, the use of induced pluripotent stem cells (iPSCs), which are produced from adult cells and have the ability to differentiate into any type of cell, is being investigated by researchers. iPSCs are being utilized more frequently in disease modeling and regenerative medicine as an ethically superior substitute for embryonic stem cells. Moreover, advancements in biomaterials and cell encapsulation have improved the delivery of cell therapies, allowing for controlled release and extended cell survival in the body, further enhancing therapeutic outcomes.
Section 5: Challenges and Ethical Considerations
There are several disadvantages to cell treatment, despite its potential. One major obstacle that keeps many patients from getting these treatments is their high cost. For example, the cost of a single CAR-T therapy session might reach the hundreds of thousands of dollars. Moreover, concerns remain over the long-term safety of cell therapies, particularly in the case of stem cell-based treatments where tumor growth or immunological rejection may occur. Using embryonic stem cells raises further ethical questions. The use of embryonic stem cells in some research, despite the availability of iPSCs as an alternative, raises ethical concerns over the destruction of embryos for medical research. Overcoming these challenges will be necessary for cell therapy to be used successfully and widely.
Conclusion
Cell therapy is revolutionizing medicine by offering cutting-edge treatments for diseases that were previously considered incurable. From the ground-breaking application of CAR-T cell therapy in the treatment of cancer to the use of stem cells for regenerative purposes, the potential applications of cell therapy are diverse and constantly developing. As research advances, new methods like as CRISPR gene editing and the generation of induced pluripotent stem cells (iPSCs) are being used to improve the precision, safety, and efficacy of these treatments. These advancements are creating opportunities for more targeted and customized therapies, allowing for carefully created interventions to meet each patient’s specific needs.
Despite the enormous potential of cell therapy, there are numerous challenges facing it. In order for adoption to become more widespread, concerns about long-term safety, high treatment costs, and ethical dilemmas—particularly in relation to the use of embryonic stem cells—must be addressed. To make these innovative treatments accessible to more people while maintaining stringent safety and efficacy standards, changes must also be made to the legal and healthcare systems.
We should expect greater advancements in the next years as clinical trials and research continue to progress. Cell therapy has a promising future since it can treat and possibly even cure some of the most challenging illnesses. Cell therapy is a rapidly evolving field with many opportunities for innovation and discovery, making it a fundamental aspect of modern medicine for researchers and medical professionals.
References
- June CH, O’Connor RS, Kawalekar OU, Ghassemi S, Milone MC. CAR T cell immunotherapy for human cancer. Science. 2018 Mar 23;359(6382):1361-1365. doi: 10.1126/science.aar6711. PMID: 29567707.
- Trounson A, McDonald C. Stem Cell Therapies in Clinical Trials: Progress and Challenges. Cell Stem Cell. 2015 Jul 2;17(1):11-22. doi: 10.1016/j.stem.2015.06.007. PMID: 26140604.
- Maude SL, Teachey DT, Porter DL, Grupp SA. CD19-targeted chimeric antigen receptor T-cell therapy for acute lymphoblastic leukemia. Blood. 2015 Jun 25;125(26):4017-23. doi: 10.1182/blood-2014-12-580068. Epub 2015 May 21. PMID: 25999455; PMCID: PMC4481592.
- Cyranoski D. CRISPR gene-editing tested in a person for the first time. Nature. 2016 Nov 24;539(7630):479. doi: 10.1038/nature.2016.20988. PMID: 27882996.
- Lindvall O, Kokaia Z. Stem cells in human neurodegenerative disorders–time for clinical translation? J Clin Invest. 2010 Jan;120(1):29-40. doi: 10.1172/JCI40543. PMID: 20051634; PMCID: PMC2798697.
- Eyquem J, Mansilla-Soto J, Giavridis T, van der Stegen SJ, Hamieh M, Cunanan KM, Odak A, Gönen M, Sadelain M. Targeting a CAR to the TRAC locus with CRISPR/Cas9 enhances tumour rejection. Nature. 2017 Mar 2;543(7643):113-117. doi: 10.1038/nature21405. Epub 2017 Feb 22. PMID: 28225754; PMCID: PMC5558614.
- Schuster SJ, Bishop MR, Tam CS, Waller EK, Borchmann P, McGuirk JP, Jäger U, Jaglowski S, Andreadis C, Westin JR, Fleury I, Bachanova V, Foley SR, Ho PJ, Mielke S, Magenau JM, Holte H, Pantano S, Pacaud LB, Awasthi R, Chu J, Anak Ö, Salles G, Maziarz RT; JULIET Investigators. Tisagenlecleucel in Adult Relapsed or Refractory Diffuse Large B-Cell Lymphoma. N Engl J Med. 2019 Jan 3;380(1):45-56. doi: 10.1056/NEJMoa1804980. Epub 2018 Dec 1. PMID: 30501490.
- Lo B, Parham L. Ethical issues in stem cell research. Endocr Rev. 2009 May;30(3):204-13. doi: 10.1210/er.2008-0031. Epub 2009 Apr 14. PMID: 19366754; PMCID: PMC2726839.




