Exploring the Potential of Quinolones in Treating Genitourinary Cancers
Abstract
Quinolones, traditionally known for their efficacy as broad-spectrum antibiotics, have recently received attention for their potential role in cancer treatment, particularly in genitourinary cancers such as prostate and bladder cancers. This review explores the dual function of quinolones, focusing on their ability to inhibit DNA synthesis and repair mechanisms, which are critical for both bacteria and cancer cells. The high concentrations of quinolones that can be achieved in urine make them particularly promising for use in bladder cancer treatment, as they can effectively target cancer cells in the bladder. However, challenges such as low accumulation of prostate tissue and the risk of antibiotic resistance require further study. Strategies such as enhanced drug administration and combination therapy were proposed to optimize its anticancer effect. While the current findings are promising, the future of quinolones in oncology will depend on extensive clinical studies to determine their safety and efficacy. This review highlights the need to continue to explore quinolones as potential adjuncts to cancer treatment, offering a new therapeutic approach that takes advantage of their favorable pharmacokinetics and relatively low toxicity.
Introduction to Quinolones and Genitourinary Cancers
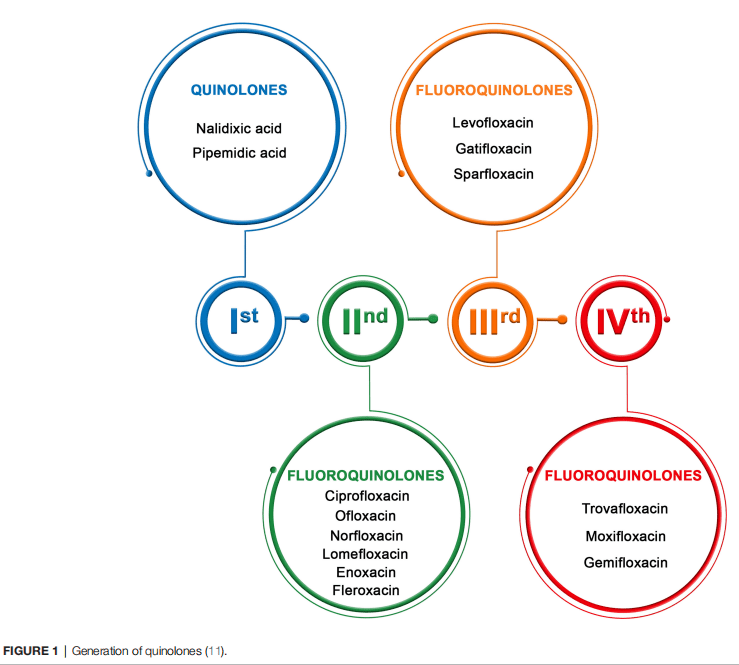
Quinolones are chemotherapeutics discovered in 1962. The application of this drug is limited due to the short time of action and fastoccurring bacterial resistance.The quinolones and their derivatives are synthetic antibiotics that show antibacterial activity against Gram (+) and Gram (–) bacteria. The mechanism of their bactericidal activity is based on the inhibition of topoisomerase II or IV complex with DNA, which consequently leads to cell death.Due to the high concentrations of these antibiotics achievable in the urine and prostate, they are widely used in the treatment of genitourinary tract infections.
Prostate cancer (PCa) is the most frequent type of cancer amongmen and second around the globe. High PCa occurrence is a global problem; it is the most frequently diagnosed cancer in men in over one-half of countries globally. Bladder cancer (BCa) is a much less common type of cancer than PCa. Worldwide, it is the 10th most common type ofcancer. Prostate and bladder cancers are among the most common cancers in men and pose a major challenge to global health.
Increases in the use of fluoroquinolones in recent years have resulted in the gradual development of fluoroquinolone resistance among gram-negative bacilli. The researchers further analyzed the anticancer properties of quinolones in combination. Studies have shown that quinolones may inhibit the growth of cancer cells by interfering with DNA synthesis in bacteria and human cellsThis dual effect offers a possibility for quinolones to be used as an adjunct to cancer treatment. Targeting bladder cancer, the high urinary concentrations of these drugs can enhance their effectiveness against cancer cells.
As research progresses, quinolones may become an important tool in the treatment of genitourinary cancers. To fully investigate its potential and address any risks of its use in cancer treatment, scientists need further clinical studies.
How Quinolones Work: Beyond Bacteria
Quinolones are a class of synthetic antibiotics primarily known for their effectiveness in treating bacterial infections. These drugs function by targeting bacterial DNA gyrase and topoisomerase IV, enzymes crucial for DNA replication and repair. By inhibiting these enzymes, quinolones prevent bacteria from replicating and ultimately cause bacterial cell death. This mechanism has made quinolones a go-to option for treating various infections, particularly those of the urinary and respiratory tracts.
Interestingly, the same mechanism that makes quinolones effective against bacteria also opens up the possibility for their use in cancer treatment. Research has shown that quinolones can inhibit similar topoisomerases in eukaryotic cells, including human cells. This inhibition can lead to disruptions in DNA replication and repair within cancer cells, potentially resulting in cell cycle arrest and apoptosis (programmed cell death). The ability of quinolones to interfere with eukaryotic topoisomerases has sparked interest in their potential use as anticancer agents, particularly in genitourinary cancers such as prostate and bladder cancers.
The effectiveness of quinolones against cancer cells has been demonstrated in various studies, particularly in vitro, where these drugs have shown the ability to inhibit the growth of cancer cells. For instance, ciprofloxacin and levofloxacin have been studied for their effects on cancer cell lines, with some promising results. However, the exact mechanisms through which quinolones exert their anticancer effects are still being studied, and more research is needed to fully understand their potential in this new role.
In conclusion, while quinolones are traditionally used as antibiotics, their ability to interfere with DNA processes in eukaryotic cells positions them as promising candidates for cancer therapy. This dual functionality highlights the versatility of quinolones and underscores the need for further research into their potential anticancer applications.
Quinolones in Bladder Cancer Treatment
Bladder cancer is a major health problem, especially in developed countries, where it is the tenth most common cancer in the world. Traditional treatment options for bladder cancer include surgery, chemotherapy, and immunotherapy. However, the high recurrence rate after initial treatment for bladder cancer warrants exploration of other therapeutic strategies. Quinolones, a class of antibiotics, as potential agents for bladder cancer treatment is an emerging area of research.
Quinolones, particularly ciprofloxacin, have shown the ability to inhibit the growth of bladder cancer cells in preclinical studies. These antibiotics reach high concentrations in the urine, which is particularly advantageous for the treatment of bladder cancer because cancer cells are directly exposed to high concentrations of the drug in the bladder. This high local concentration enhances the cytotoxic effect of quinolones on bladder cancer cells, making them a promising option for bladder cancer treatment.
Studies have shown that ciprofloxacin can induce apoptosis (programmed cell death) and inhibit cell proliferation in bladder cancer cell lines T24 and J82. The effectiveness of ciprofloxacin is thought to be related to its ability to interfere with DNA replication and repair mechanisms within cancer cells, which is similar to the effect of ciprofloxacin on bacterial cells. In addition, the acidic environment of the bladder in combination with high concentrations of ciprofloxacin may enhance its cytotoxic effects, making it more effective in killing cancer cells while reducing the risk of systemic side effects.
Despite these promising findings, the use of quinolones in the treatment of bladder cancer is still in the experimental stage. Clinical trials are needed to confirm its efficacy and safety in humans. In addition, there are concerns about the development of antibiotic resistance, which may limit the long-term use of quinolones in cancer treatment. However, their potential as adjuvant therapy for bladder cancer, especially in reducing recurrence rates, warrants further investigation.
Balancing Benefits and Risks in the Use of Quinolones for Cancer Treatment
Quinolones are broad-spectrum antibiotics that have attracted considerable interest for their potential role in cancer therapy due to their ability to target both bacteria and eukaryotic cells. While the idea of quinolones for cancer treatment is promising, particularly for genitourinary cancers, the benefits and harms must be carefully weighed.
One of the major advantages of quinolones is their proven efficacy as antibiotics, and there is increasing evidence of their anticancer properties. For example, quinolones such as ciprofloxacin have shown the ability to induce apoptosis and inhibit cancer cell proliferation in various in vitro studies. They are particularly effective against bladder cancer when present in high concentrations in urine. In addition, their relatively low toxicity and well-known pharmacokinetics make them attractive drug candidates for cancer therapy.
However, the use of quinolones in the treatment of cancer carries significant risks. A major concern is the possibility of antibiotic resistance, which may be exacerbated by the increased use of these drugs in oncology. This could lead to the emergence of more challenging resistant strains. In addition, quinolones can disrupt the natural microbiota, particularly in the gut and urinary tract, which may negatively affect the immune system and overall health. Such interference may also reduce the effectiveness of immunotherapy, a key component of modern cancer care.
Given these concerns, it is critical to use quinolones carefully in the clinical setting, ensuring that their application is evidence-based and tailored to the individual needs of the patient. Continued research is needed to optimize their role in cancer care, including exploration of combination therapies that increase efficacy while minimizing the risk of resistance and other side effects.
Conclusion and Future Outlook for Quinolones in Cancer Treatment
Quinolones have long been valued for their effectiveness as antibiotics, but recent research has unveiled their potential as anticancer agents, particularly in the treatment of genitourinary cancers such as prostate and bladder cancers. As our understanding of these drugs deepens, it is becoming clear that quinolones could play a significant role in cancer therapy, either as standalone treatments or in combination with other therapeutic agents.
The promise of quinolones lies in their ability to target DNA synthesis and repair mechanisms, which are crucial processes not only in bacteria but also in rapidly dividing cancer cells. This dual action provides a compelling rationale for their use in oncology. In bladder cancer, for example, the high concentration of quinolones in urine suggests that these drugs could be particularly effective in targeting cancer cells localized in the bladder. Similarly, although more challenging due to lower tissue concentrations, quinolones could also be used in prostate cancer, possibly through enhanced delivery methods or in combination with other treatments.
Before quinolones can be widely adopted in cancer therapy, several challenges must be addressed. Key concerns include the risks of antibiotic resistance and disruption of the microbiota, which require careful management. Additionally, the limited clinical data on quinolones’ efficacy as cancer treatments necessitates further research. This research should focus on optimizing dosing, understanding their molecular mechanisms, and exploring combination therapies. While quinolones show promise as a new approach in cancer treatment, their future in oncology depends on ongoing research and careful clinical application, potentially offering new hope for patients with genitourinary cancers and beyond.




