Immune Checkpoint Inhibitors
Abstract
Immune checkpoints are molecules in the body’s immune system that protect against the overactivation of T cells, causing inflammatory damage, and so on. By taking advantage of this characteristic of the human immune system, tumor cells can inhibit the response of the human immune system by overexpressing immune checkpoint molecules, thus avoiding human immune surveillance and killing, thus promoting the growth of tumor cells. Immune checkpoint inhibitor therapy mainly inhibits the activity of the immune checkpoint and reactivates the immune response of T cells to tumor cells, thus achieving the anti-tumor effect, which makes it a new anti-tumor strategy.
What are Immune Checkpoint Inhibitors
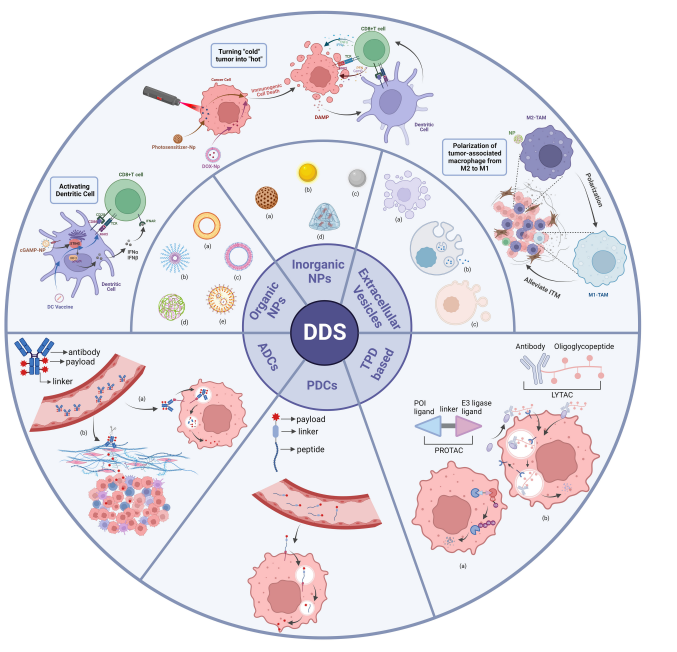
Tumor immunotherapy is a therapeutic strategy to stimulate and increase the immune function of the body through various means, and finally to control and kill tumor cells through the body’s immune system. Tumor immunotherapy can be divided into active immunotherapy and passive immunotherapy according to whether it actively promotes the body’s anti-tumor immune response. Active immunotherapy mainly includes therapeutic tumor vaccines, passive immunotherapy includes antibody-drug therapy, adoptive immune cell therapy, cytokine therapy, and so on. Among the antibody-drug therapy, immune checkpoint inhibitor therapy has received the most attention at present.
Immune checkpoints are molecules in the body’s immune system that protect against the overactivation of T cells, causing inflammatory damage, and so on. By taking advantage of this characteristic of the human immune system, tumor cells can inhibit the response of the human immune system by overexpressing immune checkpoint molecules, thus avoiding human immune surveillance and killing, thus promoting the growth of tumor cells. Immune checkpoint inhibitor therapy mainly inhibits the activity of the immune checkpoint and reactivates the immune response of T cells to tumor cells, thus achieving the anti-tumor effect, which makes it a new anti-tumor strategy.
What is CTLA-4
Cytotoxic T lymphocyte-associated antigen 4 (CTLA-4) is mainly expressed in activated T cells or killer (NK) cells. CTLA-4 is an activation-induced homologous dimer glycoprotein receptor on T cells that can interact with the CD80/CD86 ligand on the surface of antigen-presenting cells. When combined with CD80/CD86, CTLA-4 can reverse-regulate T cell activation, resulting in a decline in T cell response. Therefore, blocking CTA-4 can reactivate the immune response of T cells to play an anti-tumor role. FDA in 2011 approved anti-CTLA-4 antibodies ipilimumab for the treatment of metastatic melanoma; this marked the beginning of a new era for cancer immunotherapy. Ipilimumab is a fully humanized IgG1 monoclonal antibody that effectively blocks the binding of CTLA-4 to its ligand. Early clinical trials have proved that it is well tolerated and effective in patients with advanced cancer. However, 60% of patients were found to have immune-related adverse reactions (irAEs) in subsequent clinical applications. The most common irAEs were cutaneous and gastrointestinal toxicity, including rash, pruritus, diarrhea, colitis, etc. It can be found that CTLA-4 inhibitors are highly toxic, which is closely related to the wide expression of CTLA-4 in vivo.
Relatively speaking, small molecule inhibitors have the advantages of eliminating immunogenicity, low production cost, high stability, good tumor penetration, easy oral administration, etc., and are expected to become a viable alternative to antibody inhibitors as immune checkpoint inhibitors. By analyzing the protein model of CTLA-4 and using computer-aided drug design technology, researchers obtained more than 2000 compounds that may have good binding ability to the target. Several molecules with good medicinal properties were further selected based on the five rules of class drugs. The compound ZINC04515726 with the strongest binding ability was obtained by the calculation of binding capacity. The experimental data of ADME preliminarily proved the feasibility of its patent medicine. The gastrointestinal absorption of the compound is high indicating that it can easily be absorbed by the GIT, which is favorable for their respective biological transport toward CTLA-4. Likewise, its inability to pass through the blood-brain barrier (BBB) could indicate its suitability for targeting cancer cells not found in the central nervous system (CNS). The above results indicate that ZINC04515726 is expected to be a good small molecule inhibitor against CTLA-4.
What is PD1& PD-L1
Programmed cell death protein 1 (PD-1, also known as CD279) is one of the most widely studied inhibitory checkpoint molecules expressed on the surface of mature T lymphocytes to counteract with the T-cell receptor (TCR) signaling via ligation of its ligand, programmed death-ligand 1 (PD-L1, also known as CD274 or B7-H1), leading to T cell exhaustion, characterized by loss of differentiation, proliferation, cytokine production, and cytolytic activity. After T cells enter the tumor microenvironment, PD-1 weakens the response of T cells at the later stage of activation.
PD-L1 has been found to be widely overexpressed in various types of cancer cells, including melanoma, lymphoma, glioblastoma, breast cancer, lung cancer, bladder cancer, kidney cancer, and ovarian cancer, and is believed to play key roles for cancer cells to escape from immune surveillance. Blockade of the PD-L1 /PD-1 axis can reactivate the anergy T cells and therefore has been considered as a major strategy to overcome the immune resistance of cancer cells. Studies have shown that only when PD-1 binds to PD-L1 can it produce significant inhibitory effect on T cells through mTOR and PI3K/AKT pathway.
So far, there have been six monoclonal antibodies targeting PD-L1/PD-1 axis approved by the US Food and Drug Administration (FDA) and have achieved great success in treating multiple types of cancers, especially the advanced and refractory ones. However, there are also some disadvantages associated with the antibody agents, such as immunogenicity, instability, high cost, limited modes of administration, and low penetration into tissues, urging the need for developing small molecular inhibitors of the PD-L1/PD-1 signaling pathways.
Most recently, two small molecule antagonists (BMS-1001 and BMS-1166) that directly and selectively disrupt the association between PD-1 and PD-L1 have been identified. According to previous reports, these BMS compounds bind to and induce PD-L1 dimerization thereby preventing canonical interactions with PD-1. Mechanistically, these compounds bind to a PD-L1 monomer (APD-L1) and facilitate the recruitment of another PD-L1 monomer (BPD-L1) to form an ABPD-L1 thereby blocking interactions with the naturally occurring PD1. In other words, the ability of these compounds to induce the formation of PD-L1 dimers underlies its antagonistic functions since PD-L1 dimerization presents a hurdle for the canonical interactions between PD-L1 monomers and its intrinsic ligand, PD-1, resulting in the activation of T cells.
The compound YWN-00640 was attached to the surface of PD-L1 dimer by molecular docking using computer-aided drug design technology. Connection result display, YWN-00640 binds well in the hydrophobic binding site of the dimeric PD-L1, the distal biphenyl and central phenyl group of CH1 formed π-π interactions with 2 different TYR56 from the two chains of PD-L1, which may stabilize the complex upon ligand binding. Furthermore, the piperidine nitrogen and the carboxylic acid moiety of the hydrophilic side chain (tail group), and the oxygen of the trifluoromethoxy group of YWN-00640 forms 3 hydrogen bonds with ASP122, LYS124 and ARG125 of PD-L1, respectively, which might provide further stabilization to the PD-L1/inhibitor complex. The hydrogen bonds, along with the hydrophobic π-π interactions offered by the biphenyl moiety, may account for the excellent binding affinity of CH1 to PD-L1, leading to high anti-PD-1/PD/L1 activity.
What is VISTA
V-domain Ig suppressor of T-cell activation (VISTA) is a novel negative checkpoint ligand that is homologous to PD-L1 and suppresses T-cell activation. Unlike PD-1 and CTLA-4, VISTA is mostly expressed in bone marrow cells and granulocytes, with low expression in mouse and human T cells. VISTA is highly expressed on myeloid cells and Foxp3+CD4+ regulatory cells, but not on tumor cells within the tumor microenvironment (TME). VISTA blockade altered the suppressive feature of the TME by decreasing the presence of monocytic myeloid-derived suppressor cells and increasing the presence of activated dendritic cells within the tumor microenvironment. In addition, VISTA blockade impaired the suppressive function and reduced the emergence of tumor-specific Foxp3+CD4+ regulatory T cells. Functionally, VISTA inhibitors can slow tumor overgrowth, especially when combined with a tumor vaccine.
In 2016, researchers published phase I trials date of CA-170, a small-molecule inhibitor against PD-L1/L2 and VISTA, with low nanomolar potencies for the treatment of advanced solid tumors and lymphomas. CA-170 is also undergoing phase II clinical trials for lung cancer, head and neck/oral cavity cancer, MSI-H positive cancers and Hodgkin lymphoma in India. According to the preclinical in vitro and in vivo data, CA-170 demonstrated dose-dependent enhancement in the proliferation of PD-L1, PD-L2, and VISTA-inhibited T lymphocytes, and exhibited antitumor effects similar to those of antibodies, including tumor shrinkages and prolonged stable disease without adverse effects. PD-1-IN-17 as derivative of CA-170 is also shown great inhibitory activity in vitro test.
VISTA modulator 6809-0223 is a new VISTA inhibitor, which has good binding effects on the surface of VISTA protein. It showed great antitumor effects in mouse melanoma inhibition experiments, which can be used in the subsequent development of VISTA inhibitors.
What is IDO
Indoleamine2,3-dioxygenase (IDO) is the rate-limiting enzyme of tryptophan metabolism and a key immunosuppressive enzyme that regulates tumor immune response. IDO-expressing cells are found constitutively in many tissues, including the epididymis, gut, lymph nodes, spleen, thymus, and lungs. In these tissues, IDO regulates local inflammation and immune response to foreign or uncommon non-pathological antigens. IDO activity is also found at the maternal-fetal interface where it has a critical role in inducing maternal immune tolerance to the paternally-derived allogeneic antigens expressed by the fetus. The overexpression of IDO has been detected in melanoma, prostate cancer, pancreatic cancer, breast cancer, and other tumors. The activity of IDO leads to a decrease in tryptophan in the tumor microenvironment and an increase in the amount of canine uridine, which binds primarily to the aryl hydrocarbon receptor (AhR), an intracellular soluble receptor of immune cells that leads to the proliferation of regulatory T cells. Therefore, an increase in the amount of canine urine can inhibit the activation, differentiation, and activity of effector T cells. However, tumor cells can achieve immunosuppression or immune escape by activating the IDO activity of antigen-presenting cells. Cancer was found to increase the activity of macrophages and the level of peripheral canine urine. Canine uridine can cross the blood-brain barrier and cause neuroinflammatory microglia to produce quinolinic acid, which is a known antagonist of the aspartate receptor (NMDA) and 7-nicotinic acetylcholine (7-nACh) receptors and can damage nerves. Therefore, higher IDO activity is closely associated with poorer cancer treatment outcomes, just as fatigue is also associated with neurological disorders. Indoximod is a clinical investigational drug candidate for the treatment of cancer intended to be administered in combination with other cancer therapies that involve stimulation of an immune response to the tumor, such as cancer immunotherapy, chemotherapy, or radiotherapy. Indoximod has been tested in human cancer clinical trials in combination with different chemotherapeutic and immunotherapeutic agents, such as docetaxel, paclitaxel, gemcitabine, nab-paclitaxel, temozolomide, idaurubicin, daunorubicin, cytarabine, ipilimumab, pembrolizumab, nivolumab, sipuleucel-T, and vaccines. As a prodrug molecule of Indoximod, NLG802 is selected as a candidate drug for clinical development due to its pharmacological properties such as higher oral utilization. In a melanoma model, NLG802 significantly enhanced the antitumor response of tumor-specific PMEL-1T cells.
What is PARP14
The transcription factor STAT6, induced by IL-4 or IL-13 binding to IL-4Ra, plays a critical role in IgE production, T cell differentiation to functional subsets, chemokine secretion by lung epithelial cells, and in promoting pathological levels of mucus production. transcriptional cofactors that modulate the function of STAT6 in these diverse processes identified poly(ADPribose) polymerase (PARP)14 (alternatively termed ARTD8) as an interaction partner that binds to the activation domain of STAT6 but not the IFN-γ-induced transcription factor STAT1. Moreover, the domain of PARP14 homologous to mammalian PARP1 and to ADP-ribosyltransferases (ARTs) encoded by bacterial exotoxins is enzymatically active. Unlike the members of the PARP gene family that function as processive polymerases, PARP14 is thought to transfer only one or a few ADP-ribose (ADPr) moieties onto protein acceptor sites. RBN012759 is a cell permeable, soluble probe that achieves continuous target coverage in mice with oral dosing. RBN012759 inhibits MARylation in primary human macrophages and demonstrates robust stabilization of endogenous PARP14 in cells and in vivo. Inhibition of PARP14 with RBN012759 reverses IL-4driven protumor gene expression in macrophages and induces an inflammatory mRNA signature similar to immune checkpoint inhibitor therapy in primary human tumor explants. These data support an immune suppressive role of PARP14 in tumors and suggest potential utility of PARP14 inhibitors in the treatment of cancer.
What is TNKS
The Wnt/β-catenin pathway is known to regulate cell proliferation, stem cell renewal, and tissue differentiation. When Wnt binds to the Frizzled receptor, key transcription co-factor β-catenin forms a complex with transcription factor T-cell factor (TCF) and transcribes downstream genes. Wnt/β-catenin pathway activation is regulated by the degradation of β-catenin by the β-catenin destruction complex consisting of adenomatous polyposis coli (APC), Axin, glycogen synthase kinase 3 (GSK3β) and casein kinase (CK1) α. In cancer patients, due to mutation or the overexpression of the Wnt/ β-catenin pathway-related gene, this pathway is often activated and considered to contribute to malignant transformation, tumor progression, and resistance to conventional cancer therapy. Consequently, it is hypothesized that targeting the Wnt/β-catenin pathway may be utilized to directly inhibit tumor cell proliferation or cancel resistance to conventional therapy. One important discovery was that tankyrase (TNKS) can be a target molecule for Wnt/β-catenin pathway regulation. TNKS1 and TNKS2 belong to the poly (ADP-ribose) polymerase (PARP) family and catalyze the formation of poly-ADP-ribose chain from β-nicotinamide adenine dinucleotide (β-NAD+). In the Wnt/β-catenin pathway, Axin is poly (ADP-ribosyl) ated (PARsylated) by TNKS leading to ubiquitination by RNF146 for degradation. Thus, the application of a TNKS inhibitor causes the accumulation of Axin in the cell and promotes β-catenin degradation, which leads to selective Wnt/β-catenin pathway inhibition. Thus, TNKS inhibitors may be useful in cancer immunotherapy for attracting CD8+ T cells to tumors and overcoming resistance to ICIs. Researchers discovered dual-pocket binding K-476, which was demonstrated to be a highly potent and selective TNKS inhibitor and to show higher Wnt/βcatenin pathway inhibitory activity in comparison to K-756. K-756 interacts with TNKS mainly by the stacking of the benzene ring of dimethoxy quinazoline with His1048 and Phe1035, and the binding of the benzene ring of quinazoline2-one to the hydrophobic area of TNKS. The introduction of 3-cyano-4-fluorophenyl moiety in K-476 resulted in the acquisition of additional interactions with Ser1068 and Gly1032 of the nicotinamide pocket. These interactions are almost equivalent to those of the pyrimidine-4-one moiety scaffold of XAV939, which partly explains the high potency of K-476. The TNKS inhibitory activity of K-476 is 360 times more potent than the original lead compound, K-756. We consider it noteworthy that the 3-cyano-4-fluorophenyl group of K- 476 bound to the nicotinamide pocket of TNKS without causing any conformational or structural rearrangements within the K-756-based moiety or the residues in the ADP ribose binding pocket. After a series of tests, K-476 has the potential to be a safe and attractive therapeutic agent that enhances the efficacy of ICIs.