Is ticagrelor really superior to clopidogrel?
Abstract
As a new type of non-thienopyridine ADP receptor antagonist, ticagrelor can reversibly bind to P2Y12 receptor to exert the anti-platelet aggregation effect without enzyme metabolism activation, and its antiplatelet effect will not change due to individual differences. As a third-generation antiplatelet drug, ticagrelor has been used in clinical treatment in recent years, showing obvious advantages. It can inhibit platelet activity, prevent platelet adhesion and aggregation, and reduce the incidence of thrombotic events in patients with cardiovascular disease. Related studies have shown that in addition to antiplatelet, ticagrelor also enhances plaque stability and improves vascular endothelial function, and plays a positive role in promoting the treatment of patients with coronary heart disease.
Overview of acute coronary syndrome
Acute coronary syndrome (ACS) is a common cardiovascular disease. ACS refers to the acute ischemic syndrome of the heart caused by the rupture or erosion of coronary atherosclerotic plaques, resulting in complete or incomplete occlusive thrombosis in the lumen. It is a serious type of coronary atherosclerotic heart disease. This disease has a high mortality rate and a rapid course of the disease, which has become an important cause of death in non-communicable diseases worldwide.
At present, the treatment of ACS mainly includes drug therapy, surgical treatment, and interventional therapy. To improve the symptoms and prognosis of ACS, ACS drug treatment is divided into antiplatelet drugs, anticoagulant drugs, angiotensin II receptor antagonists, angiotensin-converting enzyme inhibitors, β receptor blockers, and statins. In recent years, ticagrelor has been widely used as a new antiplatelet drug in the treatment of ACS.
Overview of ticagrelor
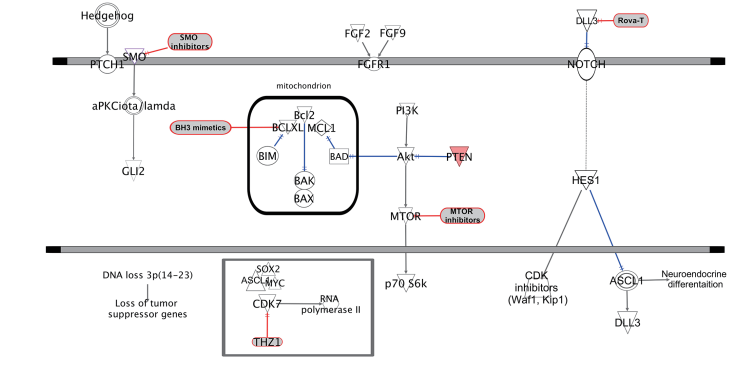
Ticagrelor (TGL) is a novel antiplatelet drug that reversibly binds to P2Y12 receptor and is mainly used for ACS and percutaneous coronary intervention. The TGL chemical structure is shown in Figure 1. Ticagrelor can directly bind to ADP receptor and can reversibly bind to it, reduce the level of cAMP in platelets and further inhibit platelet activation and aggregation. After taking ticagrelor, it can be transformed into an active metabolite AR-C124910XX by CYP3A4 and CYP3A5 in the liver. Relevant studies have shown that AR-C124910XX can also bind to P2Y12 receptors reversibly and inhibit platelet aggregation. In addition to inhibiting platelet aggregation by binding to P2Y12 receptor, the mechanism of ticagrelor can also inhibit adenosine uptake by affecting the function of balanced nucleoside transporter-1, thereby increasing extracellular adenosine concentration. Studies have shown that adenosine increases coronary blood flow; inhibition of platelet activation reduces platelet aggregation; triggers or mediates ischemic preconditioning to reduce myocardial perfusion injury. At the same time, the increase in adenosine level can also activate the G protein-coupled adenosine receptor of the C fiber of the pulmonary vagus nerve, which leads to the symptoms of bleeding and dyspnea.
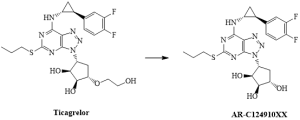
Figure 1. The structural formula of ticagrelor and its active metabolite AR-C124910XX
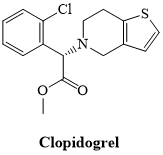
Figure 2. The structural formula of Clopidogrel
Advantages of Ticagrelor
Quick onset
Clopidogrel is a precursor drug, which needs to be activated by two steps of metabolism under the action of the P450 enzyme in the liver to produce effective active metabolites. Ticagrelor can directly act on P2Y12 receptor without conversion. The plasma concentration increases rapidly after oral administration, takes effect at 0.5 h, and reaches the peak at 2 h. ONSET/OFFSET study showed that ticagrelor took effect more quickly and achieved effective platelet inhibition rate. After ticagrelor and clopidogrel loading doses were given respectively, the inhibition of platelet aggregation (IPA) in ticagrelor group reached 41 % at 0.5 h, 98 % of subjects had IPA > 70 % at 2 h, while the IPA in clopidogrel group was 31 % at 2 h.
Strong efficacy
After clopidogrel enters the blood circulation, about 85 % is hydrolyzed into inactive products by esterase, and 15 % is transformed into active products after metabolism in the liver. The protease encoded by CYP2C19 gene is the key enzyme in its metabolic process. Several studies have shown that clopidogrel resistance is associated with CYP2C19 gene polymorphism. CYP2C19 has multiple alleles, among which CYP2C19 * 2 and * 3 are loss-of-function alleles. People carrying this allele have a reduced ability to resist platelet aggregation, resulting in high platelet reactivity. As a non-precursor drug, ticagrelor can directly bind to P2Y12 receptor to inhibit platelet activation and aggregation without metabolic activation in the liver, avoiding the reduction of the antiplatelet effect caused by CYP2C19 gene polymorphism. And the active metabolite AR-C124910XX of ticagrelor also has the effect of anti-platelet aggregation. Therefore, ticagrelor has a stronger antiplatelet effect than clopidogrel.
Effectively improve cardiac function
Compared with clopidogrel, ticagrelor can inhibit platelet aggregation more efficiently in a shorter period, thus reducing cardiac hypoperfusion, cardiac dysfunction, and reduced activity endurance caused by coronary artery insufficiency. Ticagrelor can also increase the concentration of adenosine in plasma by inhibiting cell uptake of adenosine. Studies have shown that the increase in plasma adenosine concentration has a protective effect on the heart. The mechanism may be related to the activation of A2 and A3 receptors. The binding of adenosine to the A2 receptor of the vascular endothelium can expand the coronary artery and increase the coronary blood flow. Adenosine can also inhibit platelet activation by activating A2 receptors. It is a potent platelet aggregation inhibitor in platelet-rich plasma and can reduce thrombosis by reducing platelet aggregation. At the same time, adenosine can protect the myocardium by activating A2a and A3 receptors, trigger or mediate ischemic preconditioning, and reduce myocardial perfusion injury. The above mechanisms can reduce the myocardial ischemia of patients, improve the level of cardiac function, improve the endurance of patients, and reduce the reperfusion injury caused by acute myocardial ischemia. Therefore, ticagrelor is more effective in improving cardiac function than clopidogrel.
Adverse reaction
Compared with clopidogrel, ticagrelor had a slight increase in some minor bleeding and non-CABG-related bleeding, but there was no difference in major bleeding and fatal bleeding. And this risk decreases rapidly with the rapid recovery of platelet function after discontinuation of ticagrelor. For patients who need surgery, platelet function can be quickly restored after drug withdrawal, and surgical treatment can be performed earlier and safer.
Although ticagrelor has side effects such as dyspnea, bradyarrhythmia, and increased serum uric acid and creatinine levels, most of these adverse reactions are transient, tolerable, and can be terminated by discontinuing treatment.
Summary
Ticagrelor is the first oral, directly acting antiplatelet drug that can reversibly bind to P2Y12 receptor. It inhibits platelet aggregation faster, stronger, and more consistently. Its use does not need to consider whether the patient has CYP2C19 gene polymorphism. The rapid onset of ticagrelor allows us to quickly achieve antiplatelet effects after taking medicine for some emergency patients. Today, the PLATO study has concluded that the use of ticagrelor in ACS patients will benefit more and reduce mortality more effectively than clopidogrel, which has not been seen for a long time.