Letrozole: Pharmacology, Therapeutic Efficacy, and Clinical Considerations
Abstract
Letrozole, a third-generation aromatase inhibitor, plays a critical role in the treatment of hormone receptor-positive breast cancer in postmenopausal women. By selectively inhibiting the aromatase enzyme, Letrozole effectively reduces estrogen levels, which is essential for slowing the progression of estrogen-responsive breast cancers. This medication has demonstrated superior efficacy in extending disease-free survival and reducing recurrence rates compared to other endocrine therapies, such as tamoxifen. While Letrozole offers substantial benefits, its use is associated with potential adverse effects, including osteoporosis and cardiovascular risks, necessitating careful management and monitoring. Ongoing research aims to enhance the therapeutic efficacy of Letrozole through new formulations, combination therapies, and personalized treatment approaches based on genetic profiles, positioning it as a cornerstone in breast cancer therapy.
Introduction
Letrozole, a third-generation aromatase inhibitor, represents a significant advancement in the treatment of hormone receptor-positive breast cancer among post-menopausal women. Developed to block the aromatase enzyme crucial for the estrogen biosynthesis pathway, particularly in adipose tissue post-menopause, Letrozole significantly reduces estrogen levels. This reduction is vital for slowing the progression of estrogen-responsive breast cancers which thrive on estrogen.
The introduction of Letrozole has revolutionized the management of breast cancer by providing a highly effective option with potentially fewer side effects compared to previous therapies. Estrogen plays a pivotal role in the growth and development of many breast tumors. By mitigating estrogen production, Letrozole starves these cancer cells of their primary growth stimulus. This mechanism of action makes it particularly effective in treating cancers that exhibit estrogen receptor positivity.
Letrozole’s impact on breast cancer treatment is profound. Its ability to decrease estrogen levels translates into a tangible retardation of tumor progression and a noticeable improvement in patient survival rates. Studies have shown that Letrozole not only improves outcomes in terms of cancer recurrence but also extends overall survival among breast cancer survivors. Its role in the adjuvant therapy of post-menopausal women with hormone receptor-positive breast cancer is now well-established, making it a cornerstone of breast cancer treatment protocols worldwide.
Mechanism of Action
Letrozole operates through a fascinating mechanism due to its selective inhibition of the aromatase pathway. Unlike earlier generations of aromatase inhibitors, Letrozole does not indiscriminately inhibit all sources of estrogen but selectively targets the aromatase enzyme. This enzyme is responsible for a key step in the synthesis of estrogens from androgen precursors. By binding to the enzyme’s heme group, Letrozole effectively blocks this conversion, leading to a significant reduction in estrogen levels.
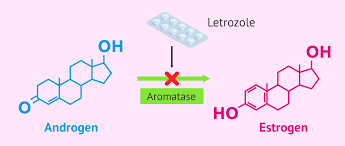
Fig.1 Letrozole action mechanism
This selective action is beneficial for reducing the systemic side effects often associated with estrogen depletion, such as severe menopausal symptoms and bone density loss. Furthermore, the precision of Letrozole’s mechanism allows for higher drug efficacy, reducing tumor size and proliferation more effectively than many other treatments. The ability of Letrozole to minimize estrogen production makes it particularly useful in treating breast cancers that are stimulated by this hormone.
In clinical settings, this means that Letrozole can be administered even in advanced stages of breast cancer, providing hope and improved outcomes for patients who may have limited treatment options. The drug’s action is crucial not only in treating existing cancer but also in preventing the recurrence of tumors, thereby playing a pivotal role in the long-term management of breast cancer.
Pharmacodynamics and Pharmacokinetics
The pharmacodynamics of Letrozole demonstrate its potent ability to suppress plasma estrogen levels with minimal off-target effects, which is crucial for its effectiveness in treating breast cancer. The drug’s action leads to a dramatic reduction in the circulating levels of estrogen, which is directly correlated with a decrease in the progression and recurrence of hormone-sensitive breast tumors.
Pharmacokinetically, Letrozole is characterized by excellent absorption and bioavailability, which means that it is efficiently taken up into the bloodstream after oral administration. This leads to peak plasma concentrations within a couple of hours, making it rapidly effective following dosing. Letrozole also exhibits a relatively long half-life, which supports its once-daily dosing regimen. This pharmacokinetic profile facilitates ease of use and adherence to the treatment schedule, which is vital for the success of long-term therapy.
Metabolism of Letrozole primarily occurs in the liver, where it is transformed into an inactive metabolite that is then excreted predominantly through the kidneys. This metabolic pathway suggests that Letrozole’s use needs to be carefully monitored in patients with liver or kidney impairment to adjust dosing and prevent accumulation of the drug, which could potentially lead to toxicity. Understanding these pharmacokinetic dynamics is essential for optimizing treatment schedules and doses, particularly in patients with varying degrees of hepatic or renal function.
Therapeutic Efficacy
Letrozole’s therapeutic efficacy significantly surpasses that of earlier treatments due to its potent and selective inhibition properties. In clinical trials and real-world applications, Letrozole has demonstrated substantial benefits in extending disease-free survival and reducing recurrence rates compared to other endocrine therapies. Its effectiveness is particularly noted in the adjuvant setting, where it dramatically decreases the likelihood of cancer recurrence following primary treatment such as surgery.
Research consistently shows Letrozole’s superiority over tamoxifen, another commonly used endocrine therapy, particularly in reducing the risk of distant metastases. This is a critical consideration as distant metastases are a major cause of morbidity and mortality in breast cancer patients. Letrozole’s ability to improve overall survival and delay cancer recurrence makes it a preferred choice for long-term management of hormone receptor-positive breast cancer in post-menopausal women.
Adverse Effects
Despite its significant benefits, Letrozole is associated with a range of adverse effects, which are important for clinicians and patients to consider. Commonly reported side effects include hot flashes, joint pain, and fatigue—symptoms that are often manageable but can affect quality of life. More serious concerns arise with prolonged use, particularly related to bone health and cardiovascular risks.
Fig. 2 Precautions and side effects
Osteoporosis is a notable risk due to the prolonged suppression of estrogen, a hormone crucial for maintaining bone density. Post-menopausal women, already at risk due to natural decreases in estrogen, may experience an accelerated decline in bone density with Letrozole therapy. This necessitates routine monitoring of bone health through densitometry and the possible use of bone-strengthening agents like bisphosphonates.
Cardiovascular risks are also heightened with Letrozole due to its impact on lipid profiles. The suppression of estrogen can lead to unfavorable changes in cholesterol levels, potentially increasing the risk of cardiovascular diseases such as arteriosclerosis and heart attacks. This aspect of Letrozole therapy must be carefully managed with regular cardiovascular assessments and the integration of lipid-lowering therapies if needed.
The management of these adverse effects involves a proactive approach, including lifestyle interventions such as diet and exercise modifications, as well as pharmacological measures to counteract the negative impacts of estrogen depletion. Patient education and regular monitoring for symptoms of osteoporosis and cardiovascular changes are crucial components of comprehensive care for patients receiving Letrozole.
Comparative Analysis
When compared to other aromatase inhibitors like anastrozole and exemestane, Letrozole stands out for its improved patient outcomes, particularly in terms of survival rates and side effect profiles. Studies have demonstrated Letrozole’s efficacy not only in prolonging disease-free survival but also in minimizing the severity and occurrence of side effects typically associated with estrogen depletion.
In the neoadjuvant setting—treatment given to shrink a tumor before the main treatment—Letrozole has shown better efficacy in reducing tumor size more effectively than its counterparts. This is particularly beneficial for patients who may require surgery, as smaller tumors may allow for less invasive surgical techniques and potentially better surgical outcomes.
Letrozole’s favorable profile extends to its use in different clinical scenarios beyond the typical scope of breast cancer treatment, such as in early breast cancer and as a preventive option for high-risk patients. Its broad applicative potential makes it a versatile tool in the arsenal against hormone receptor-positive breast cancer, providing patients with a powerful option for both treatment and prevention.
Clinical Trials and Studies
The role of Letrozole continues to expand as new research and clinical trials explore its potential beyond the traditional boundaries of breast cancer treatment. One intriguing area of study is its use in treating infertility, particularly among women with polycystic ovary syndrome (PCOS). Letrozole’s ability to increase follicle-stimulating hormone (FSH) levels by reducing estrogen offers a promising therapeutic pathway for inducing ovulation in women struggling with this common endocrine disorder.
Recent trials have shown that Letrozole may be more effective and less detrimental to the endometrial lining than clomiphene citrate, a commonly used drug in fertility treatments. These findings suggest that Letrozole could become a preferred treatment option in reproductive medicine, offering hope to countless women facing difficulties in conceiving naturally.
Further studies are examining the application of Letrozole in combination therapies, particularly in resistant forms of cancer where monotherapy has failed. By combining Letrozole with other therapeutic agents, researchers hope to overcome resistance mechanisms and improve outcomes for patients with advanced stages of cancer.
Future Directions
Continued research into Letrozole includes the development of new formulations that can mitigate side effects or enhance its efficacy. Ongoing studies are exploring how to combine Letrozole with other therapeutic agents to counteract resistance mechanisms commonly seen in advanced cancer stages. Additionally, genetic research is uncovering biomarkers that can predict responses to Letrozole, potentially ushering in an era of more personalized treatment approaches.
This burgeoning field of pharmacogenomics holds the promise of optimizing Letrozole therapy based on individual genetic profiles, thereby maximizing efficacy while minimizing adverse effects. Such tailored treatment strategies could revolutionize how hormone receptor-positive breast cancer is managed, making therapy more effective and less burdensome for patients.
Conclusions
Letrozole remains a cornerstone in the treatment of hormone receptor-positive breast cancer in postmenopausal women. Its precise mechanism of action and robust efficacy profile make it a preferred choice in both adjuvant and neoadjuvant therapies. However, the management of side effects and the ongoing development of complementary therapies are crucial to maximizing patient outcomes and enhancing the quality of life.
As research continues to advance, Letrozole’s role may expand further, solidifying its status as a vital component of breast cancer therapy. The future holds the promise of even greater improvements in care, with Letrozole at the forefront of innovative approaches to treatment and prevention.




