Prucalopride: A Breakthrough in Treating Chronic Idiopathic Constipation and Gastroparesis
Abstract
Prucalopride, a selective serotonin (5-HT4) receptor agonist, has shown significant clinical efficacy in treating chronic idiopathic constipation (CIC) and gastroparesis. This blog post outlines prucalopride’s mechanism of action, its effectiveness in improving bowel movement frequency and alleviating gastrointestinal symptoms, and its common adverse effects. By selectively stimulating the 5-HT4 receptors, prucalopride enhances gastrointestinal motility through neurotransmitter modulation. Clinical trials have demonstrated substantial improvements in symptoms and quality of life for patients with CIC and gastroparesis. The potential for prucalopride to treat other gastrointestinal disorders, such as IBS-C, is also explored. Future research, including the use of isotopes, will further elucidate prucalopride’s long-term safety, efficacy, and expanded therapeutic applications.
Introduction to Prucalopride
Functional gastrointestinal disorders, such as chronic idiopathic constipation (CIC) and gastroparesis, significantly impact patients’ quality of life and contribute to increased healthcare costs. CIC is characterized by persistent difficulty in bowel movements, leading to symptoms like straining, hard stools, and a sensation of incomplete evacuation. Gastroparesis, on the other hand, involves delayed gastric emptying without any mechanical obstruction, causing nausea, vomiting, bloating, and early satiety. These conditions often require long-term management and can be challenging to treat effectively.
Prucalopride is a novel treatment option that has garnered attention for its efficacy in addressing these functional gastrointestinal disorders. It is a highly selective serotonin (5-HT4) receptor agonist that enhances gastrointestinal motility by stimulating the release of neurotransmitters, such as acetylcholine, which facilitate bowel movements and gastric emptying. This specificity minimizes the risk of cardiovascular side effects associated with earlier non-selective serotonin receptor agonists.
Developed and approved for use in several countries, prucalopride has shown promise in clinical trials. For chronic idiopathic constipation, studies have demonstrated that prucalopride significantly improves bowel movement frequency and alleviates associated symptoms. Patients treated with prucalopride experienced an increase in spontaneous complete bowel movements (SCBMs) per week, which is a critical measure of treatment efficacy.
In the context of gastroparesis, prucalopride has been shown to accelerate gastric emptying and reduce gastroparesis symptoms. This makes it a valuable therapeutic option for patients who do not respond adequately to conventional treatments. By improving gastrointestinal motility, prucalopride helps manage symptoms and enhances the overall quality of life for patients suffering from these debilitating conditions.
Clinical Efficacy of Prucalopride
Prucalopride has demonstrated significant clinical efficacy in treating chronic idiopathic constipation (CIC) and gastroparesis, offering a promising solution for patients who have not found relief with conventional treatments.
Effectiveness in Treating Chronic Idiopathic Constipation
Clinical trials have consistently shown that prucalopride significantly improves bowel movement frequency and alleviates symptoms associated with CIC. In several randomized, double-blind, placebo-controlled studies, patients treated with prucalopride reported a substantial increase in spontaneous complete bowel movements (SCBMs) per week compared to those receiving a placebo. For instance, a 12-week trial involving 501 patients revealed that 33.3% of participants in the prucalopride group achieved ≥3 SCBMs per week, compared to just 10.3% in the placebo group. These results were statistically significant and indicate prucalopride’s robust efficacy in managing CIC.
The typical dosage for prucalopride ranges from 2 to 4 mg/day, and it has been found effective across different populations, including the elderly. The drug’s ability to improve the number of bowel movements and enhance the overall symptom profile makes it a valuable option for long-term management of chronic constipation.
Effectiveness in Treating Gastroparesis
Prucalopride has also shown promise in the treatment of gastroparesis, a condition characterized by delayed gastric emptying. In clinical studies, prucalopride has been found to significantly accelerate gastric emptying and improve gastroparesis symptoms. For example, a four-week double-blind crossover trial with 15 patients demonstrated that prucalopride significantly increased bowel movement frequency and accelerated gastric emptying compared to placebo. These findings suggest that prucalopride can effectively manage gastroparesis symptoms, providing an alternative for patients who do not respond to other treatments.
Common Adverse Effects
While prucalopride is generally well-tolerated, common adverse effects include headache, nausea, diarrhea, and abdominal pain. These side effects are typically mild and transient, occurring primarily at the start of treatment. Despite these side effects, the overall safety profile of prucalopride supports its use in treating CIC and gastroparesis.
In conclusion, prucalopride’s clinical efficacy in improving bowel movement frequency and symptom relief in CIC and gastroparesis patients makes it a valuable therapeutic option. Its well-tolerated nature and effectiveness across different patient populations highlight its potential as a standard treatment for these challenging gastrointestinal disorders.
Mechanism of Action and Adverse Effects
Prucalopride’s effectiveness in treating chronic idiopathic constipation (CIC) and gastroparesis can be attributed to its unique mechanism of action as a selective serotonin (5-HT4) receptor agonist. Understanding how prucalopride works at the molecular level helps to explain its clinical benefits and potential side effects.
Mechanism of Action
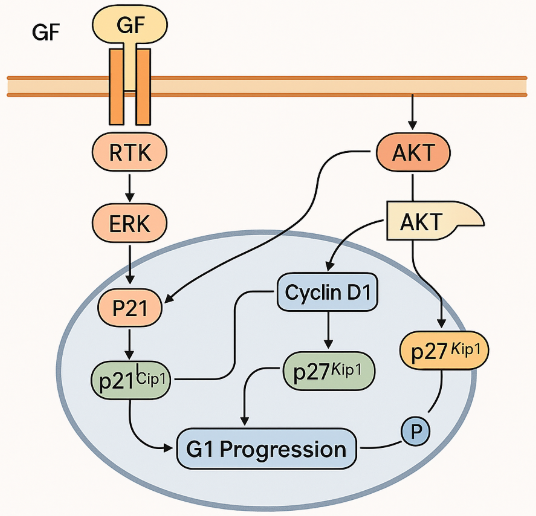
Prucalopride functions by selectively stimulating the 5-HT4 receptors, which are abundantly present in the gastrointestinal (GI) tract, specifically in the myenteric plexus, enterochromaffin cells, and smooth muscle cells. These receptors play a critical role in modulating GI motility.
When prucalopride binds to 5-HT4 receptors, it enhances the release of neurotransmitters, particularly acetylcholine. Acetylcholine promotes muscle contractions in the GI tract, facilitating the advancement of luminal contents through coordinated contractions of the longitudinal muscle and relaxation of the circular muscle layers. This activity helps to normalize bowel movements and improve gastric emptying, making prucalopride effective in treating both CIC and gastroparesis.
Prucalopride’s high affinity for 5-HT4 receptors ensures that it does not significantly interact with other serotonin receptors, which reduces the risk of adverse cardiovascular effects that were observed with earlier non-selective serotonin receptor agonists like tegaserod and cisapride.
Common Adverse Effects
Despite its benefits, prucalopride can cause some adverse effects, which are generally mild and transient. The most commonly reported side effects include headache, nausea, diarrhea, and abdominal pain. These symptoms are typically more pronounced at the beginning of the treatment and tend to diminish with continued use.
Headache: This is the most frequently reported adverse effect and may be due to the central nervous system activity of the drug.
Nausea: Often mild and transient, nausea occurs as the body adjusts to the medication.
Diarrhea: While prucalopride is designed to enhance GI motility, it can sometimes lead to excessive bowel movements, resulting in diarrhea.
Abdominal Pain: This side effect is usually mild and can be managed with dose adjustments if necessary.
Clinical trials have shown that these adverse effects are generally well tolerated. For example, in a study by Camilleri et al. (2008), the incidence of these side effects was higher in the prucalopride group compared to the placebo group, but they were not severe enough to warrant discontinuation of the treatment in most cases.
Overall, prucalopride’s selective mechanism of action and manageable side effect profile make it a viable option for patients with CIC and gastroparesis, offering significant improvements in GI motility and symptom relief.
Potential Applications and Future Research (Including Isotopes)
Prucalopride, a selective serotonin (5-HT4) receptor agonist, has shown promise beyond its current approved uses in treating chronic idiopathic constipation (CIC) and gastroparesis. This section explores potential applications, the role of isotopes in research, and future directions for studying prucalopride.
Potential Applications Beyond Current Uses
Prucalopride’s efficacy in improving gastrointestinal motility suggests that it could be beneficial for other gastrointestinal disorders. One potential application is in treating irritable bowel syndrome with constipation (IBS-C). IBS-C shares symptoms with CIC, such as infrequent bowel movements and abdominal discomfort. Although prucalopride is not currently approved for IBS-C, its mechanism of action and positive outcomes in CIC make it a candidate for future research in this area.
Additionally, prucalopride may be helpful for patients with overlapping conditions such as concurrent gastroparesis and CIC. This dual efficacy could simplify treatment regimens for patients suffering from multiple gastrointestinal motility disorders, providing a comprehensive solution with a single medication.
Role of Isotopes in Research
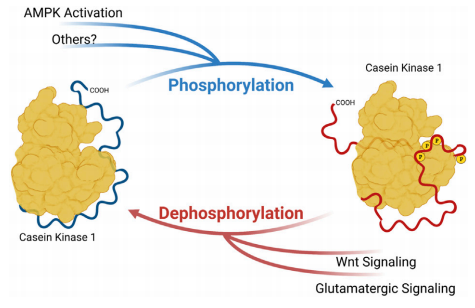
Isotopes play a critical role in clinical research, particularly in studying the pharmacokinetics and pharmacodynamics of drugs like prucalopride. By using isotopes, researchers can track the distribution and metabolism of prucalopride in the body with high precision. This helps in understanding how the drug is absorbed, distributed, and excreted, as well as its interaction with different tissues.
For instance, radioactive isotopes can be used in imaging studies to visualize the drug’s movement through the gastrointestinal tract. These studies can provide valuable insights into the specific regions of the GI tract that prucalopride affects, thereby enhancing our understanding of its mechanism of action and potential side effects.
Future Research Directions
Future research on prucalopride should focus on several key areas:
Long-term Safety and Efficacy: While current studies show prucalopride is effective in the short term, long-term studies are needed to confirm its safety and sustained efficacy over extended periods.
Comparative Studies: Direct comparisons between prucalopride and other treatments for CIC and gastroparesis can help establish its relative benefits and drawbacks.
Isotopic Studies: Continued use of isotopes in research can provide deeper insights into the drug’s pharmacological profile, helping to optimize dosing regimens and minimize side effects.
Expanded Indications: Clinical trials investigating prucalopride for IBS-C and other related conditions could expand its therapeutic applications, offering relief to a broader patient population.
By addressing these research areas, we can better understand prucalopride’s full potential and optimize its use in treating various gastrointestinal disorders.
References
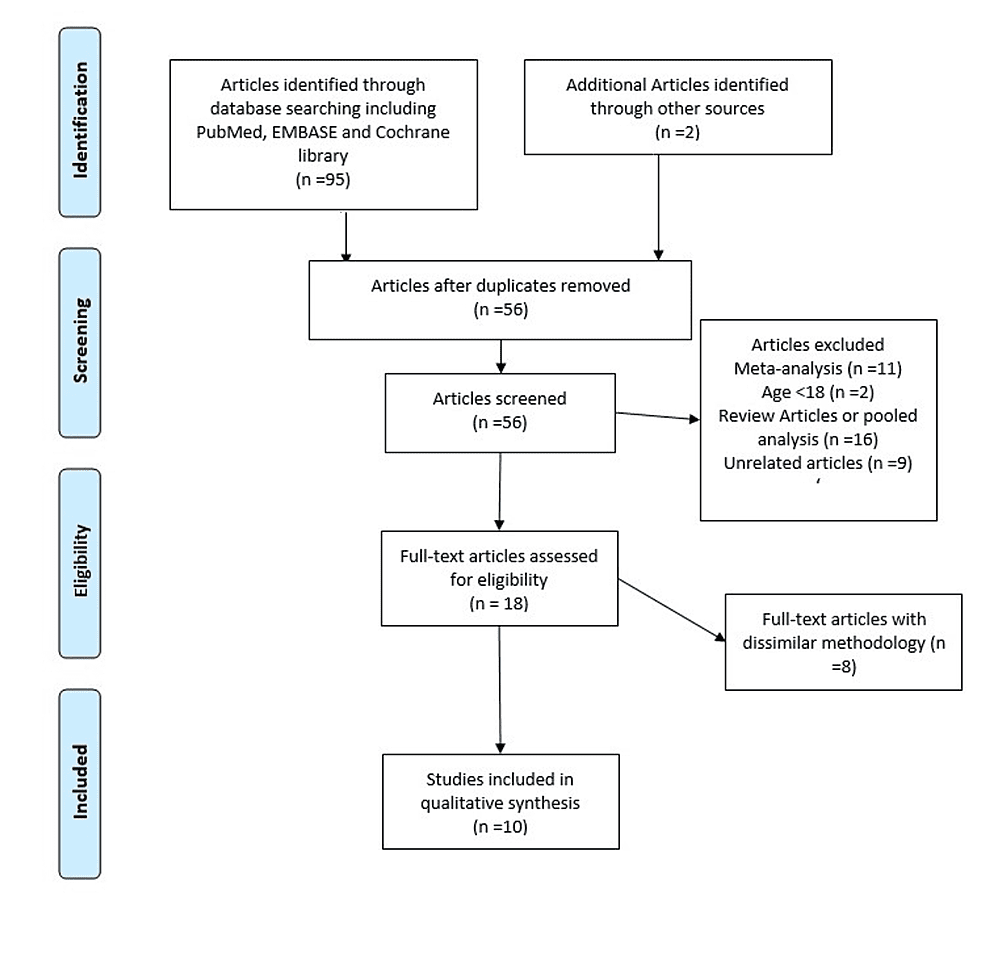
- Ali, H., Pamarthy, R., & Sarfraz, S. (2021). Role of Prucalopride in Treating Functional Constipation and Gastroparesis: A Systemic Review. Cureus, 13(4), e14306.
- Ford, A. C., Moayyedi, P., Lacy, B. E., et al. (2014). American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. American Journal of Gastroenterology, 109, S2-26.
- Quigley, E. M., Vandeplassche, L., & Kerstens, R. (2009). Clinical trial: the efficacy, impact on quality of life, and safety and tolerability of prucalopride in severe chronic constipation—a 12-week, randomized, double-blind, placebo-controlled study. Alimentary Pharmacology & Therapeutics, 29(3), 315-328.
- Camilleri, M., Kerstens, R., Rykx, A., & Vandeplassche, L. (2008). A placebo-controlled trial of prucalopride for severe chronic constipation. New England Journal of Medicine, 358(22), 2344-2354.
- Andrews, C. N., Woo, M., Buresi, M., et al. (2021). Prucalopride in diabetic and connective tissue disease-related gastroparesis: randomized placebo-controlled crossover pilot trial. Neurogastroenterology & Motility, 33(4), e13958.
- Ke, M., Zou, D., Yuan, Y., et al. (2012). Prucalopride in the treatment of chronic constipation in patients from the Asia-Pacific region: a randomized, double-blind, placebo-controlled study. Neurogastroenterology & Motility, 24(11), 999-e541.
- Yiannakou, Y., Piessevaux, H., Bouchoucha, M., et al. (2015). A randomized, double-blind, placebo-controlled, phase 3 trial to evaluate the efficacy, safety, and tolerability of prucalopride in men with chronic constipation. American Journal of Gastroenterology, 110(5), 741-748.
- De Maeyer, J. H., Lefebvre, R. A., & Schuurkes, J. A. (2008). 5-HT4 receptor agonists: similar but not the same. Neurogastroenterology & Motility, 20(2), 99-112.
- Tack, J., van Outryve, M., Beyens, G., Kerstens, R., & Vandeplassche, L. (2009). Prucalopride (Resolor) in the treatment of severe chronic constipation in patients dissatisfied with laxatives. Gut, 58(3), 357-365.