Revolutionizing Breast Cancer Treatment: The Emergence of New Estrogen Receptor Therapies
Abstract
Breast cancer remains one of the most common and deadly cancers affecting women worldwide. The estrogen receptor (ER) has long been a target for therapy, given its critical role in many breast cancers. Traditional therapies, such as selective estrogen receptor modulators (SERMs) and aromatase inhibitors (AIs), have made significant strides in treating ER-positive breast cancer. However, resistance to these therapies presents ongoing challenges. This blog post explores the evolution of breast cancer treatment, focusing on the emergence of advanced therapies like Selective Estrogen Receptor Degraders (SERDs), Complete Estrogen Receptor Antagonists (CERANs), Selective Estrogen Receptor Covalent Antagonists (SERCAs), and Proteolysis Targeting Chimeras (PROTACs). We discuss the mechanisms behind therapy resistance, the latest clinical trial results for new ER-targeting drugs, and the promising future of these treatments in enhancing patient outcomes. With a spotlight on oral selective ER degraders and the potential of personalized medicine, this post highlights the shift towards more effective and manageable treatments that aim to improve both the efficacy and quality of life for patients battling breast cancer.
Introduction to Breast Cancer and Estrogen Receptor Targeting
Breast cancer remains a leading cause of morbidity and mortality among women worldwide, affecting millions each year. The estrogen receptor (ER), a pivotal player in many breast cancer cases, has been the focus of treatment strategies for decades. ER-positive breast cancers, which express estrogen receptors, often respond well initially to therapies like tamoxifen and aromatase inhibitors that target estrogen signaling. However, the development of resistance to these treatments poses significant challenges, often leading to treatment failure and disease progression.
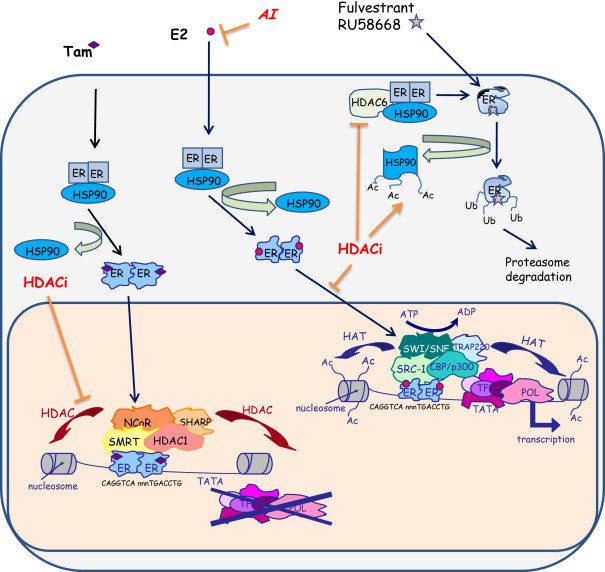
Traditional treatments such as tamoxifen, classified as selective estrogen receptor modulators (SERMs), and aromatase inhibitors, which reduce estrogen production, have been the cornerstone of breast cancer therapy. Tamoxifen blocks the estrogen receptor in breast cells, preventing estrogen from driving cancer growth, whereas aromatase inhibitors reduce the level of estrogen itself. Despite their effectiveness, a significant number of patients eventually develop resistance to these therapies. The resistance mechanisms are complex, involving genetic changes in the estrogen receptor itself or alterations in other signaling pathways that bypass the receptor’s control.
This pressing issue highlights the need for novel therapeutic strategies that can either enhance the effectiveness of current treatments or offer new avenues to circumvent resistance mechanisms. The latest advancements in estrogen receptor targeting involve a more nuanced approach, including the development of drugs that degrade the estrogen receptor, block its activity more completely, or modify its interaction with other cellular components.
As research progresses, the hope is that these new therapies will provide more durable responses in patients and lead to better outcomes. The commitment to understanding the biology of ER-positive breast cancer and overcoming the challenges of resistance is crucial for developing more effective treatments for this widespread disease.
Emerging Therapies in Estrogen Receptor Targeted Treatment
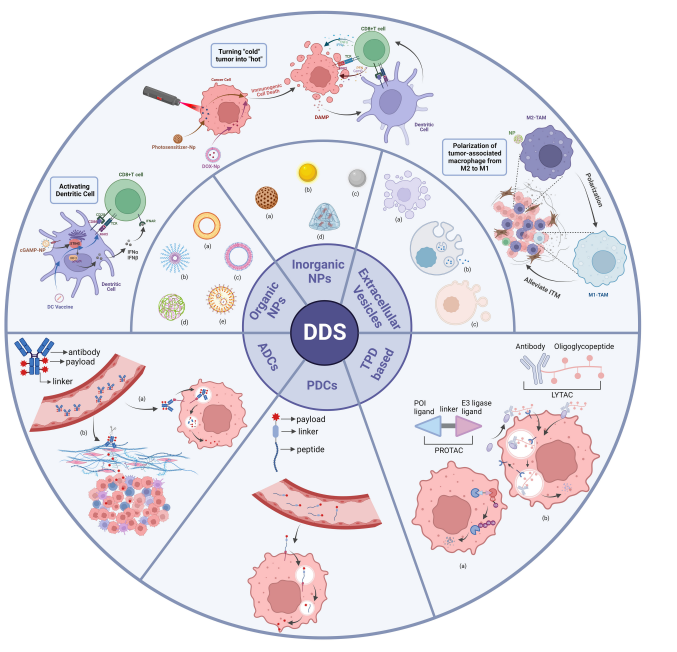
The landscape of breast cancer treatment is evolving with the development of innovative therapies that promise to outpace traditional treatments. Among the most promising are Selective Estrogen Receptor Degraders (SERDs), Complete Estrogen Receptor Antagonists (CERANs), Selective Estrogen Receptor Covalent Antagonists (SERCAs), and Proteolysis Targeting Chimeras (PROTACs). These therapies represent a significant leap forward in our ability to target the estrogen receptor with greater precision and efficacy.
SERDs, such as fulvestrant, are designed to bind to the estrogen receptor and promote its degradation, eliminating the receptor’s presence and function. Unlike SERMs, which only block the receptor’s ability to bind estrogen, SERDs ensure that the receptor is not available to trigger any cancer-promoting signals, even in non-estrogenic pathways. This approach addresses the issue of resistance seen with SERMs, where cancer cells adapt to continue growing despite the therapy.
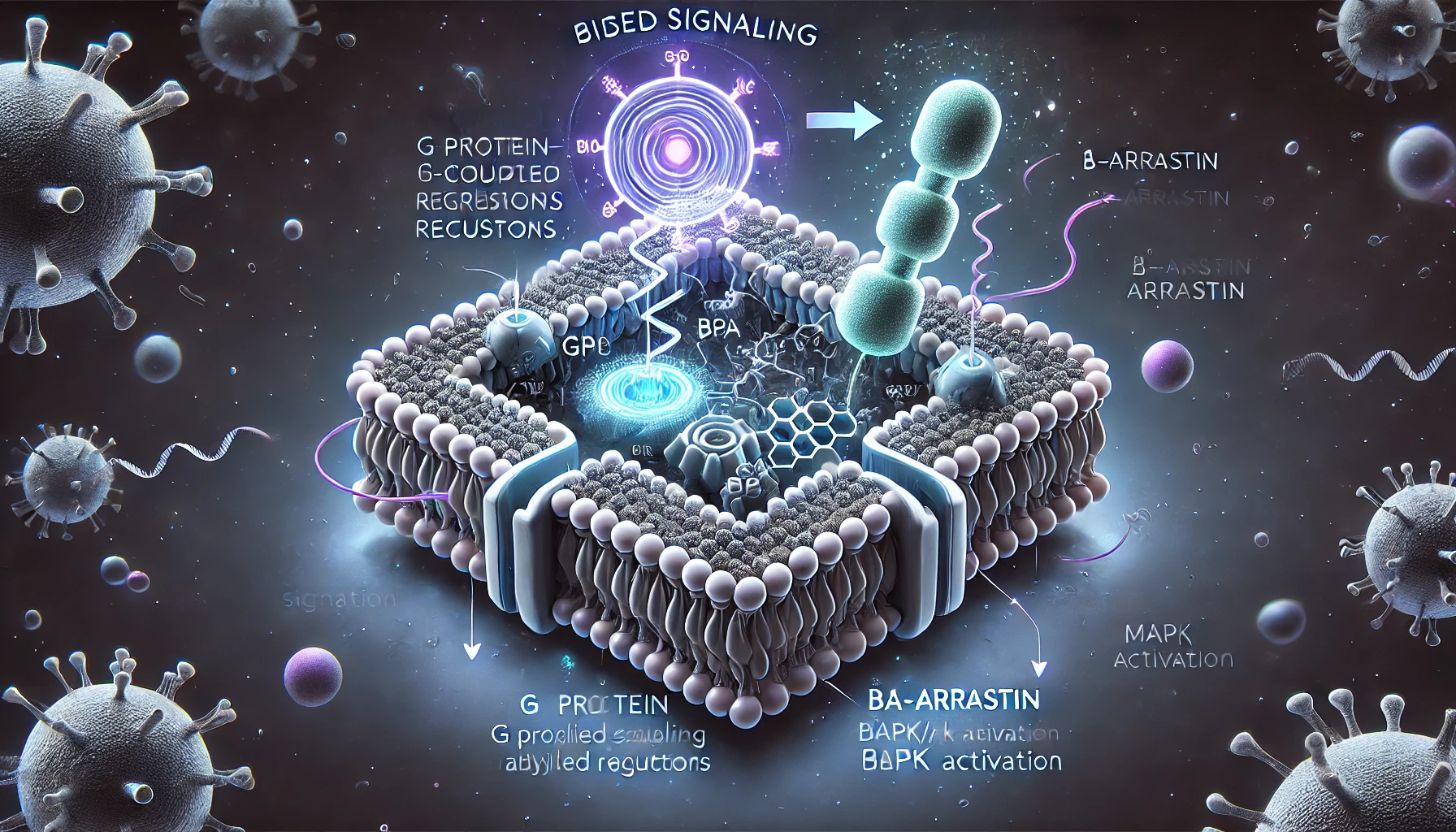
CERANs and SERCAs are newer entries in the field, offering more comprehensive ways to inhibit the estrogen receptor. CERANs block all forms of the receptor’s activity, preventing any signaling that could lead to tumor growth. SERCAs add another layer by binding covalently to the receptor, which prevents the receptor from being recycled, ensuring prolonged inhibition.
PROTACs introduce a novel mechanism by recruiting the body’s protein degradation machinery to target the estrogen receptor, leading to its destruction. This method not only blocks estrogen receptor signaling but also removes the protein entirely from cancer cells, potentially overcoming resistance mechanisms that can deactivate other forms of therapy.
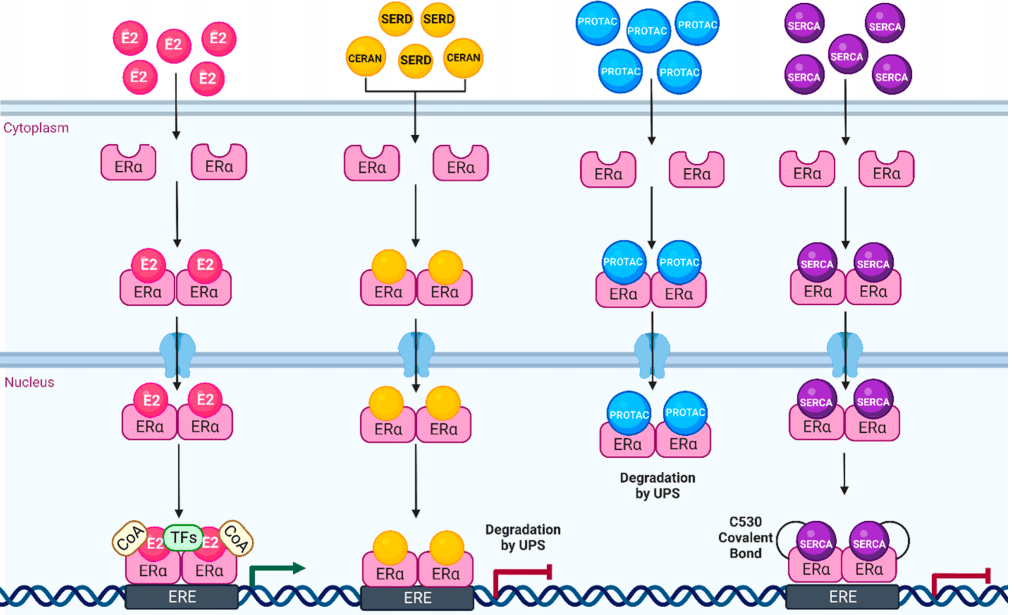
A spotlight on oral selective ER degraders highlights a shift towards improving patient compliance and quality of life. Oral SERDs bring the power of ER degradation directly into a convenient form, bypassing the need for injections and infusions typical of traditional therapies. Clinical advancements in this area have shown that these oral agents maintain the efficacy of their injectable counterparts while significantly enhancing patient comfort and adherence to treatment protocols.
Understanding Resistance in ER-Positive Breast Cancer
The battle against breast cancer is continuously evolving, with resistance to hormone therapy posing a significant challenge. Understanding the mechanisms behind resistance in estrogen receptor (ER)-positive breast cancer is crucial for developing more effective treatments. Resistance to hormonal therapies such as SERMs (Selective Estrogen Receptor Modulators) and AIs (Aromatase Inhibitors) is often multifaceted, involving genetic changes within the ER itself or adaptations in other cellular signaling pathways.
The genetic mutations in the ER gene, known as ESR1, are particularly problematic. These mutations can alter the receptor’s structure so that it is continuously active, even without estrogen. This type of mutation leads to what is known as ligand-independent activation, where the receptor promotes cancer growth without the normal hormonal trigger. Current treatments might block estrogen but do not always address these mutant, constantly active receptors.
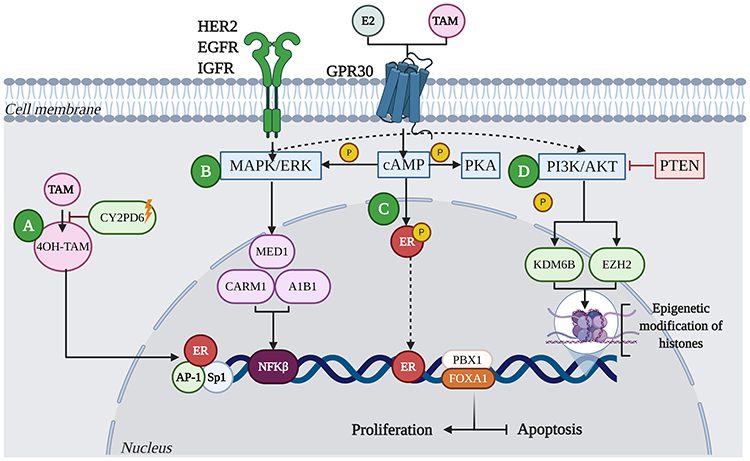
Further complicating the resistance issue is the cross-talk between ER and other growth signaling pathways. For example, even if ER signaling is blocked, pathways like PI3K/AKT or MAPK can take over, driving cancer cell proliferation. This understanding has led to the exploration of combination therapies that target multiple pathways simultaneously to prevent cancer cells from finding alternative routes to grow.
Addressing these resistance mechanisms has led to the development of next-generation SERDs and other novel compounds that can degrade the receptor or block its activity more completely. These advanced therapies aim to improve upon past treatments by ensuring that no form of the receptor—mutant or otherwise—is available to promote tumor growth.
Latest Clinical Trials and Results for ER-Targeting Drugs
As the medical community seeks to improve breast cancer outcomes, the focus on the latest clinical trials reveals significant advancements in ER-targeting drugs. These trials are crucial for evaluating the effectiveness and safety of new therapies designed to combat ER-positive breast cancer, particularly those resistant to traditional treatments.
Recent clinical trials have centered on innovative drugs such as oral selective estrogen receptor degraders (SERDs), which promise to revolutionize the treatment landscape by offering more effective management of breast cancer. These drugs, including promising candidates like elacestrant and lasofoxifene, have been shown to not only inhibit estrogen receptor activity but also degrade the receptor itself, thus reducing the chances of cancer cells developing resistance.
The results from these trials have been promising. For example, elacestrant has demonstrated significant efficacy in patients with advanced ER-positive breast cancer, showing improved progression-free survival rates compared to standard therapies. Similarly, lasofoxifene, tested in postmenopausal women, has shown effectiveness in reducing cancer recurrence rates, highlighting its potential as both a treatment and preventive measure.
However, the journey from trial to treatment is not without challenges. While these drugs show potential, they also come with side effects that need careful management. Common adverse effects reported include nausea, fatigue, and, in some cases, more severe reactions that necessitate close monitoring and management strategies to ensure patient safety.
These clinical trials not only test the efficacy and safety of new drugs but also help refine treatment protocols and identify optimal dosing strategies. They are instrumental in pushing the boundaries of what’s possible in cancer treatment, aiming for therapies that are both effective and bearable for patients.
Future Outlook in ER-Targeted Breast Cancer Treatments
As we look to the future of breast cancer treatment, the horizon is filled with innovative strategies and promising therapies that target the estrogen receptor (ER) more effectively and safely. The continuous evolution of ER-targeting drugs is not only reshaping treatment paradigms but also offering hope for longer, healthier lives for patients with ER-positive breast cancer.
The development of therapies like oral selective estrogen receptor degraders (SERDs) is particularly encouraging. These drugs provide a convenient, less invasive treatment option that could potentially replace or enhance current injectable therapies, improving patient compliance and quality of life. The ongoing research and clinical trials are expected to provide more robust data, helping to refine dosing regimens and treatment protocols, and ultimately, guide regulatory approvals.
Moreover, the integration of genomics and biomarker analysis into clinical practices is poised to transform breast cancer care. By understanding the genetic makeup of tumors, oncologists can tailor treatments more precisely, which is expected to enhance efficacy and minimize side effects. This personalized approach will be crucial in managing and eventually overcoming resistance to hormone therapies.
The future also holds potential for combination therapies that target multiple pathways simultaneously. As our understanding of cancer biology deepens, combining ER-targeting agents with inhibitors of growth factor signaling pathways or immune checkpoint inhibitors may yield synergistic effects, offering new avenues for treatment that could significantly extend patient survival and improve outcomes.
As these developments unfold, it is vital to continue supporting breast cancer research and clinical trials. The insights gained from these efforts will not only enhance our understanding of ER-positive breast cancer but also bring us closer to a future where this form of cancer can be effectively managed or even cured.