Smart Drug Delivery Systems: The Future of Cancer Immunotherapy Begins in the Tumor Microenvironment
Abstract
Recent advances in cancer immunotherapy have revealed the critical role of the tumor microenvironment (TME) in therapeutic success or failure. Traditional treatments often fall short due to poor targeting and immune resistance driven by the TME. This blog explores how smart drug delivery systems—ranging from nanoparticles and peptide-drug conjugates to cell-based carriers and oncolytic viruses—are revolutionizing cancer treatment by reprogramming the immune response. By targeting tumor-associated macrophages and inducing immunogenic cell death, these delivery strategies hold promise for transforming “cold” tumors into immunologically active ones. Despite ongoing challenges in drug stability, targeting precision, and tumor heterogeneity, the future of cancer therapy lies in personalized, programmable, and immune-enhancing delivery technologies.
Revolutionizing Cancer Treatment: The Urgent Need for Smarter Therapies
Despite decades of advances in cancer treatment, traditional therapies like chemotherapy and radiation still face major limitations. These methods often lack precision, targeting both cancerous and healthy cells alike. As a result, patients may endure severe side effects while only achieving modest therapeutic benefits. In an era where personalized medicine is gaining ground, the one-size-fits-all approach to cancer is no longer acceptable.
Cancer immunotherapy has emerged as a game-changing alternative. By harnessing the body’s own immune system to fight cancer, immunotherapies such as checkpoint inhibitors and CAR-T cell therapies have produced remarkable outcomes in specific cancer types. However, these therapies aren’t universally effective. Many tumors remain resistant due to the complex and hostile nature of the tumor microenvironment (TME), which actively suppresses immune responses and facilitates cancer progression.
To overcome these barriers, researchers are now turning to innovative drug delivery systems (DDS). These advanced platforms are designed not only to deliver drugs more accurately to tumor sites but also to modulate the TME itself—enhancing the efficacy of immunotherapies. From nanoparticles and peptide-drug conjugates to oncolytic viruses and cell-based carriers, the next generation of DDS offers a more strategic way to target cancer.
This shift toward smarter therapies is not just about improving drug performance—it’s about rethinking how we approach cancer at its biological roots. As the frontier of cancer research continues to evolve, these precision delivery technologies could be the key to unlocking more effective and less toxic treatments for patients around the world.
Understanding the Tumor Microenvironment – Friend or Foe?
When it comes to treating cancer, the tumor is only part of the problem. Surrounding it is a complex network of cells, blood vessels, and signaling molecules collectively known as the tumor microenvironment (TME). Far from being a passive bystander, the TME actively supports tumor growth, metastasis, and immune evasion. This hostile environment creates a major barrier to the success of even the most advanced immunotherapies.
The TME is often dominated by immunosuppressive cells such as tumor-associated macrophages (TAMs), myeloid-derived suppressor cells (MDSCs), and regulatory T cells (Tregs). These cells suppress the activity of cytotoxic T lymphocytes, the very immune cells responsible for destroying cancer. Additionally, the TME is characterized by abnormal vasculature, hypoxia (low oxygen levels), and acidic pH—all of which further protect the tumor from immune attack.
This immunosuppressive ecosystem contributes to what scientists refer to as “cold tumors”—tumors that lack immune infiltration and are unresponsive to immunotherapy. Reprogramming the TME to convert cold tumors into “hot” tumors that are inflamed and immunogenic is now a key objective in cancer research. Understanding and manipulating the TME has become just as important as targeting the cancer cells themselves.
Ultimately, transforming the TME from foe to friend is critical to unlocking the full potential of immunotherapy. Innovative drug delivery strategies now aim to deliver therapeutic agents that can modulate the TME directly—breaking down its defenses and paving the way for more effective, targeted treatments.
Cutting-Edge Delivery Systems – Reprogramming the Immune Response
To overcome the protective barriers of the tumor microenvironment (TME), researchers are designing smarter, targeted drug delivery systems (DDS) that can directly modulate the immune landscape within tumors. These advanced platforms aim to boost the precision, potency, and safety of cancer immunotherapy.
One of the most promising innovations is nanoparticle-based delivery, which enables the encapsulation and targeted release of drugs specifically within tumors. These nanoscale carriers can be engineered to respond to stimuli like pH or enzymes in the TME, ensuring that the payload is released exactly where it’s needed. This reduces off-target effects and enhances therapeutic efficiency.
Another strategy involves peptide-drug conjugates (PDCs)—short peptides linked to therapeutic molecules—that home in on cancer-specific receptors. By targeting overexpressed markers in the TME, PDCs offer a highly selective approach to drug delivery, improving immune modulation at the tumor site.
Additionally, cell-based DDS—such as engineered T cells, neutrophils, or macrophages—are being explored as living carriers that can deliver immunostimulatory agents deep into tumor tissue. These cells naturally navigate toward inflammation and tumors, making them ideal “Trojan horses” for therapy.
Finally, oncolytic viruses represent a dual-threat platform. They infect and lyse cancer cells while stimulating immune responses by releasing tumor antigens. Some are even engineered to carry immunomodulatory genes, further enhancing their effect within the TME.
By combining these smart delivery systems with immune-targeting agents, researchers hope to convert immune-resistant tumors into responsive ones, opening up new possibilities for combination and personalized therapies.
Targeting Tumor-Associated Macrophages and Inducing Immunogenic Cell Death
A critical challenge in cancer immunotherapy is overcoming the immune suppression within the tumor microenvironment (TME). Among the most influential players in this suppression are tumor-associated macrophages (TAMs). These immune cells, normally responsible for defending the body, are hijacked by tumors to support growth, angiogenesis, and immune evasion. In many cancers, TAMs make up a significant portion of the tumor mass and are associated with poor prognosis.
Modern drug delivery systems (DDS) offer promising strategies to reprogram or eliminate TAMs, thus removing one of the biggest obstacles to effective immunotherapy. Some approaches aim to “re-educate” TAMs, shifting them from a tumor-promoting (M2-like) state to a tumor-fighting (M1-like) state using small molecules, peptides, or nucleic acids. Other strategies target surface receptors like CSF1R or CCR2 to inhibit TAM recruitment or induce their depletion.
Equally significant is the induction of immunogenic cell death (ICD)—a form of cancer cell death that stimulates an immune response. Unlike traditional apoptosis, ICD releases damage-associated molecular patterns (DAMPs) and tumor antigens that activate dendritic cells and T lymphocytes. This process turns the tumor into an in-situ vaccine, drawing the immune system into the fight.
Advanced DDS technologies are now being designed to deliver ICD inducers—like certain chemotherapeutics or oncolytic viruses—directly into the tumor. By combining TAM modulation and ICD induction, these systems help transform immunologically “cold” tumors, which are unresponsive to therapy, into “hot” tumors that attract and activate immune cells.
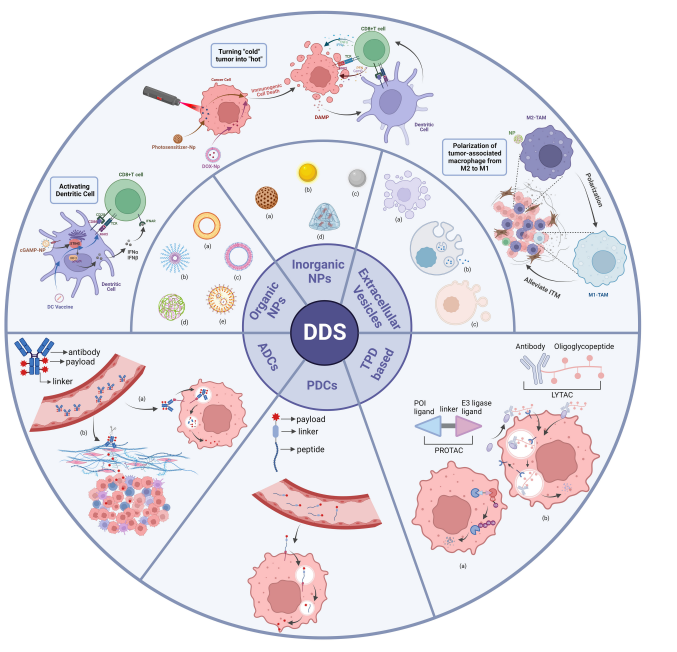
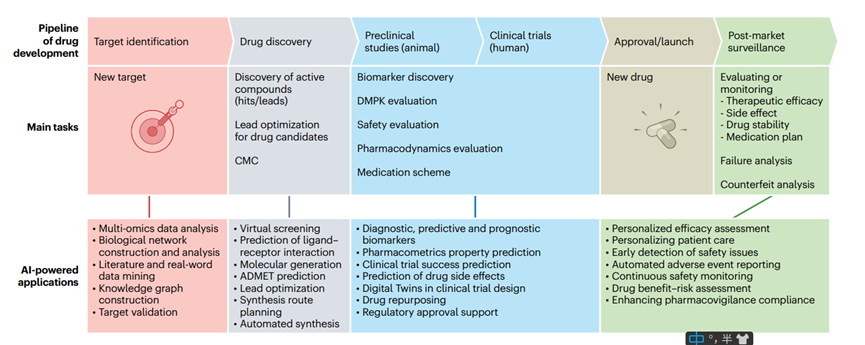
FIGURE 1. Classes of DDS. Organic NPs, inorganic NPs and extracellular vesicles are categorized as subclasses of nanoparticles-based DDS
This dual-pronged approach—reprogramming TAMs and triggering ICD—represents a paradigm shift in cancer treatment. It not only disables the tumor’s defenses but also reinvigorates the immune system, enhancing the therapeutic potential of immunotherapies across a wider range of cancers.
The Road Ahead – Challenges and Future Perspectives
The future of cancer immunotherapy is being reshaped by the development of advanced drug delivery systems (DDS). These platforms are enabling more precise, potent, and safer treatments by modulating the tumor microenvironment (TME) and enhancing immune responses. However, despite impressive progress, several key challenges must be addressed before these innovations can reach their full clinical potential.
One of the primary hurdles is drug stability and biodistribution. Many nanocarriers and peptide-drug conjugates are susceptible to degradation in the bloodstream or may accumulate in non-target tissues, leading to off-target effects. Improving the pharmacokinetics and targeting specificity of these systems remains a top research priority.
Another challenge is tumor heterogeneity. Each tumor presents a unique microenvironment, and even within the same tumor, different regions may respond differently to therapy. As a result, one-size-fits-all delivery strategies often fall short. There is growing interest in personalized DDS platforms, which can be tailored to individual tumor profiles using biomarker-driven designs.
Additionally, the immune system’s complexity poses a double-edged sword. While many delivery systems aim to activate immune responses, they must avoid triggering excessive inflammation or autoimmunity. Ensuring immune balance and long-term safety requires deeper understanding and fine-tuning of immune modulators delivered through DDS.
Looking ahead, the integration of combination therapies—such as pairing immunotherapy with chemotherapy, radiotherapy, or gene editing—offers promising avenues. Many researchers are exploring multi-functional delivery systems capable of carrying multiple agents simultaneously for synergistic effects.
Finally, advances in artificial intelligence (AI), machine learning, and omics technologies are accelerating the design of next-generation DDS. These tools can help predict optimal formulations, dosing, and timing for individual patients, moving the field closer to truly precision oncology.
In summary, while challenges remain, the future of drug delivery in cancer immunotherapy is bright. By continuing to innovate and personalize, we may soon unlock safer and more effective treatments for even the most resistant tumors.
References
Fukumura, D., & Jain, R. K. (2021). Tumor microenvironment abnormalities: Causes, consequences, and strategies to normalize. Journal of Cellular Biochemistry, 122(2), 169–180.
https://doi.org/10.1002/jcb.29542
Riley, R. S., June, C. H., Langer, R., & Mitchell, M. J. (2019). Delivery technologies for cancer immunotherapy. Nature Reviews Drug Discovery, 18(3), 175–196.
https://doi.org/10.1038/s41573-018-0006-z
Chen, D. S., & Mellman, I. (2017). Elements of cancer immunity and the cancer–immune set point. Nature, 541(7637), 321–330.
https://doi.org/10.1038/nature21349
Zhang, Y., Zhang, Z., & Zhang, D. (2023). Advanced drug delivery systems for cancer immunotherapy. Frontiers in Immunology, 15, 1328145.
https://doi.org/10.3389/fimmu.2024.1328145
Arneth, B. (2019). Tumor Microenvironment. Medicina, 56(1), 15.
https://doi.org/10.3390/medicina56010015
Quail, D. F., & Joyce, J. A. (2013). Microenvironmental regulation of tumor progression and metastasis. Nature Medicine, 19(11), 1423–1437.
https://doi.org/10.1038/nm.3394
Hinshaw, D. C., & Shevde, L. A. (2019). The Tumor Microenvironment Innately Modulates Cancer Progression. Cancer Research, 79(18), 4557–4566.
https://doi.org/10.1158/0008-5472.CAN-18-3962
Mitchell, M. J., Billingsley, M. M., Haley, R. M., Wechsler, M. E., Peppas, N. A., & Langer, R. (2021). Engineering precision nanoparticles for drug delivery. Nature Reviews Drug Discovery, 20(2), 101–124.
https://doi.org/10.1038/s41573-020-0090-8
Mastorakos, P., da Silva, A. L., Chisholm, J., Song, E., & Hanes, J. (2015). Highly compacted biodegradable DNA nanoparticles capable of overcoming the mucus barrier for inhaled lung gene therapy. Advanced Healthcare Materials, 4(10), 1417–1423.
https://doi.org/10.1002/adhm.201500122
Liu, Y., Wang, W., & Yang, J. (2020). Cell-based drug delivery systems for cancer therapy. Biomaterials Science, 8(23), 6839–6850.
https://doi.org/10.1039/D0BM01292D
Mantovani, A., Marchesi, F., Malesci, A., Laghi, L., & Allavena, P. (2017). Tumour-associated macrophages as treatment targets in oncology. Nature Reviews Clinical Oncology, 14(7), 399–416.
https://doi.org/10.1038/nrclinonc.2016.217
Najafi, M., Hashemi Goradel, N., Farhood, B., Salehi, E., Nashtaei, M. S., Khanlarkhani, N., … & Sahebkar, A. (2019). Macrophage polarity in cancer: A review. Journal of Cellular Biochemistry, 120(3), 2756–2765.
https://doi.org/10.1002/jcb.27646
Kroemer, G., Galassi, C., Zitvogel, L., & Galluzzi, L. (2022). Immunogenic cell stress and death. Nature Immunology, 23(4), 487–500.
https://doi.org/10.1038/s41590-021-01186-1
Blanco, E., Shen, H., & Ferrari, M. (2015). Principles of nanoparticle design for overcoming biological barriers to drug delivery. Nature Biotechnology, 33(9), 941–951.
https://doi.org/10.1038/nbt.3330
van der Meel, R., Sulheim, E., Shi, Y., Kiessling, F., Mulder, W. J., & Lammers, T. (2019). Smart cancer nanomedicine. Nature Nanotechnology, 14(11), 1007–1017.
https://doi.org/10.1038/s41565-019-0567-y
Marabelle, A., Kohrt, H., Sagiv-Barfi, I., Ajami, B., Axtell, R. C., Zhou, G., … & Levy, R. (2013). Depleting tumor-specific Tregs at a single site eradicates disseminated tumors. The Journal of Clinical Investigation, 123(6), 2447–2463.