Targeting PGD2 Signaling: A Promising Approach for Treating Eosinophilic Diseases and Beyond
Abstract
Prostaglandin D2 (PGD2) and its receptors, particularly DP2 (CRTH2), play a crucial role in mediating eosinophilic inflammation, which is central to the pathophysiology of various allergic and eosinophil-driven diseases, including asthma, allergic rhinitis, and atopic dermatitis. Targeting PGD2 signaling through receptor antagonists and inhibitors of PGD2 synthesis has shown promise in preclinical and clinical studies, offering new therapeutic strategies for managing these chronic conditions. This article reviews the therapeutic potential of PGD2 receptor antagonists, focusing on the current research, clinical trial outcomes, and future directions for PGD2-based therapies. It highlights the need for personalized treatment approaches, biomarker identification, and the exploration of combination therapies to improve the effectiveness of PGD2-targeted interventions. Despite challenges in optimizing drug delivery and efficacy, continued research is expected to refine these therapies and expand their use in treating both allergic and non-allergic diseases, ultimately improving patient outcomes.
Introduction to Prostaglandins and Eosinophils in Disease
Prostaglandins (PGs) are lipid compounds derived from arachidonic acid that play a critical role in the body’s inflammatory processes. These compounds are synthesized through the cyclooxygenase (COX) pathway, which results in the formation of various prostanoids, including prostaglandin D2 (PGD2), prostaglandin E2 (PGE2), and prostacyclin (PGI2). Prostaglandins act as signaling molecules, influencing numerous biological processes such as vasodilation, fever, pain modulation, and immune response regulation.
Among the many immune cells affected by prostaglandins, eosinophils stand out due to their key role in allergic and inflammatory diseases. Eosinophils are white blood cells primarily involved in combating parasitic infections, but they also play a significant part in chronic allergic inflammation. These cells release a range of pro-inflammatory mediators, including cytokines and cytotoxic proteins, which contribute to tissue damage and exacerbate diseases like asthma, rhinosinusitis, and atopic dermatitis. The function of eosinophils in these conditions is heavily influenced by prostaglandins, particularly PGD2, PGE2, and PGI2, which interact with specific receptors on the eosinophil cell surface.
PGD2, in particular, has a well-established role in mediating eosinophil migration to sites of inflammation, where it activates the DP1 and DP2 receptors. These interactions enhance eosinophil chemotaxis, cytokine release, and tissue remodeling, all of which are pivotal in the pathogenesis of allergic diseases. Conversely, PGE2 and PGI2 tend to suppress eosinophil activation, demonstrating the complex and sometimes opposing effects of prostaglandins in immune responses. The balance between these prostanoids can determine the severity of inflammation and guide potential therapeutic strategies targeting prostaglandin signaling pathways to manage eosinophil-driven diseases.
Understanding the intricate relationship between prostaglandins and eosinophils is crucial for developing more effective treatments for allergic and inflammatory diseases, offering hope for patients suffering from chronic conditions exacerbated by eosinophil activation.
The Role of Prostaglandin D2 (PGD2) in Eosinophil Activation
Prostaglandin D2 (PGD2) is a potent lipid mediator involved in the regulation of immune responses, particularly in allergic and inflammatory diseases. One of the key roles of PGD2 is its interaction with eosinophils, which are central to the pathogenesis of chronic allergic inflammation, such as asthma, rhinitis, and dermatitis. Eosinophils express specific receptors for PGD2, including the DP1 and DP2 receptors, which mediate its biological effects.
The DP2 receptor, also known as the chemoattractant receptor homologous molecule expressed on Th2 cells (CRTH2), is predominantly expressed on eosinophils. When PGD2 binds to DP2, it triggers several cellular responses, including eosinophil chemotaxis, cytokine production, and activation of various signaling pathways. PGD2-induced eosinophil migration is an essential step in the recruitment of these cells to sites of allergic inflammation, contributing to the exacerbation of diseases like asthma and allergic rhinitis. In addition to migration, PGD2 activates eosinophils to release pro-inflammatory cytokines and other mediators that promote tissue damage and further immune cell recruitment, creating a vicious cycle of inflammation.
PGD2 also interacts with the DP1 receptor, though its effects are more complex. While DP1 activation can contribute to some pro-inflammatory responses, it has been shown to inhibit other functions, such as eosinophil apoptosis, thus promoting the survival of eosinophils in inflamed tissues. This highlights the dual roles that PGD2 and its receptors play in regulating eosinophil activity. Through DP1 and DP2, PGD2 influences eosinophil function in both the early and late phases of allergic responses, and its dysregulation is linked to the severity of allergic diseases.
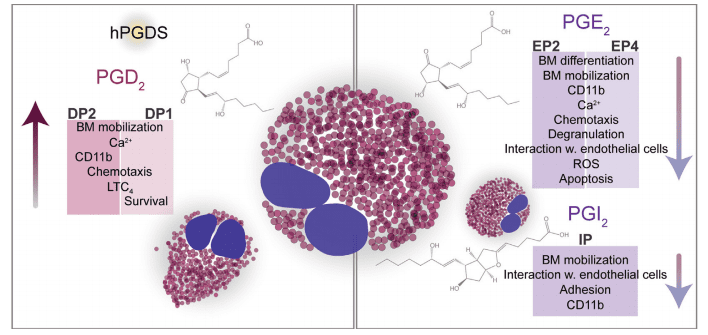
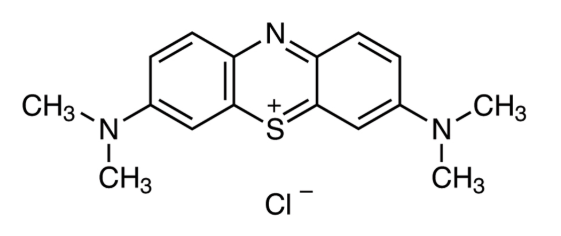
Figure 1. GD2, PGE2, and PGI2 direct the functions of eosinophils. Eosinophils express receptors for PGD2 (DP1, DP2), PGE2 (EP2, EP4), and PGI2 (IP). Via DP2
PGD2 attracts eosinophils to the site of inflammation, enhances eosinophil mobilization from the bone marrow, and upregulates CD11b expression
Given its pivotal role in eosinophil-driven inflammation, targeting the PGD2 signaling pathway offers a promising therapeutic strategy. Antagonists of DP2, for example, have shown potential in reducing eosinophil recruitment and activation in animal models, paving the way for future clinical applications in treating eosinophil-mediated diseases.
Therapeutic Potential of Targeting PGD2 Signaling
The role of prostaglandin D2 (PGD2) in regulating immune responses, particularly through its interaction with eosinophils, has made it a key target for therapeutic intervention in various allergic and inflammatory diseases. PGD2 exerts its effects on eosinophils by binding to two primary receptors, DP1 and DP2. These receptors mediate a range of cellular responses, including chemotaxis, cytokine release, and cell survival, which contribute to the pathogenesis of diseases like asthma, allergic rhinitis, and dermatitis. Therefore, targeting PGD2 signaling holds significant promise as a therapeutic approach for these conditions.
The DP2 receptor, also known as CRTH2, has garnered particular attention due to its prominent role in eosinophil recruitment and activation. In allergic diseases, elevated levels of PGD2 lead to increased eosinophil infiltration, exacerbating inflammation. Several studies have demonstrated that blocking the DP2 receptor can reduce eosinophil migration to inflamed tissues, thereby alleviating symptoms of allergic diseases. DP2 antagonists, such as timapiprant and fevipiprant, have shown promise in preclinical and clinical trials by reducing eosinophilic inflammation in asthma, allergic rhinitis, and other conditions characterized by excessive eosinophil activity.
In addition to DP2 antagonism, targeting PGD2 synthesis and metabolism offers another potential strategy. Inhibiting the enzymes responsible for PGD2 production, such as hematopoietic prostaglandin D synthase (HPGDS), can reduce the overall levels of PGD2 and its inflammatory effects. This approach may be particularly beneficial in chronic inflammatory diseases where PGD2 production is dysregulated. Furthermore, PGD2 metabolism generates several biologically active metabolites that can also influence eosinophil function. Developing selective inhibitors of PGD2 synthases and its metabolites may provide a more targeted approach to managing eosinophil-driven diseases.
Overall, targeting PGD2 signaling, through receptor antagonism or inhibition of its synthesis and metabolism, presents a promising therapeutic strategy. By modulating PGD2 activity, it may be possible to reduce eosinophil-mediated inflammation, offering new hope for patients suffering from chronic allergic and inflammatory diseases.
PGD2 Receptor Antagonists and Their Impact on Eosinophilic Diseases
Prostaglandin D2 (PGD2) plays a significant role in eosinophil recruitment and activation, particularly in allergic and inflammatory diseases. This has led to considerable interest in developing PGD2 receptor antagonists as therapeutic agents to treat conditions such as asthma, allergic rhinitis, and atopic dermatitis. The primary receptors for PGD2 on eosinophils are DP1 and DP2, with DP2 (CRTH2) being particularly involved in eosinophil migration and activation. By targeting these receptors, PGD2 receptor antagonists aim to reduce the inflammation and tissue damage caused by excessive eosinophil activity.
The DP2 receptor, in particular, has become a prominent target in the development of novel therapies for eosinophilic diseases. Antagonists of this receptor, such as timapiprant (OC-459) and fevipiprant (QAW039), have been tested in clinical trials. Studies have shown that timapiprant can significantly reduce eosinophil infiltration and improve lung function in patients with asthma. In a large clinical trial, timapiprant demonstrated favorable effects on lung function, particularly in patients with active eosinophilia. This was further supported by post-hoc analysis, which suggested that the drug was especially effective in younger patients. Similarly, fevipiprant, another DP2 antagonist, showed promise in reducing eosinophilic airway inflammation in asthma patients, particularly in those with severe, uncontrolled asthma. Although the overall results of fevipiprant trials have been mixed, its efficacy in specific subgroups, such as patients with severe eosinophilic asthma, has sparked continued interest in further investigation.
These DP2 receptor antagonists highlight the potential of targeting PGD2 signaling to treat eosinophil-driven diseases. By inhibiting the recruitment and activation of eosinophils, these drugs may reduce inflammation and alleviate symptoms in patients suffering from chronic allergic conditions. The ongoing development of PGD2 receptor antagonists, along with further clinical trials, holds promise for more effective and targeted treatments for eosinophilic diseases.
Future Directions and Conclusion
The growing understanding of prostaglandin D2 (PGD2) signaling in eosinophilic diseases has opened up new avenues for therapeutic intervention. PGD2 plays a central role in mediating the inflammatory responses seen in conditions like asthma, allergic rhinitis, atopic dermatitis, and other eosinophil-driven diseases. The therapeutic potential of targeting PGD2 receptors, particularly the DP2 receptor (CRTH2), has already been demonstrated in clinical trials with receptor antagonists such as timapiprant and fevipiprant. These studies show promise in alleviating eosinophilic inflammation and improving patient outcomes. However, further research is needed to refine these treatments and understand the full scope of PGD2’s role in other diseases, particularly non-allergic conditions like cancer and inflammatory bowel disease (IBD).
Looking ahead, one of the key areas of focus will be identifying biomarkers to predict which patients will benefit most from PGD2-targeted therapies. While DP2 antagonists have shown efficacy in reducing eosinophilic inflammation, their success varies among patients. Personalized treatment strategies that use biomarkers to identify suitable candidates could maximize therapeutic outcomes and minimize unnecessary treatments. Additionally, more research is needed to explore the broader effects of PGD2 and its metabolites in other immune cells, as well as their impact on disease progression and resolution.
Another critical area for future development is improving the pharmacokinetics of PGD2 receptor antagonists. Drugs like fevipiprant and timapiprant show efficacy, but challenges remain in ensuring their optimal absorption, distribution, and long-term effectiveness in diverse patient populations. Additionally, exploring combination therapies that target PGD2 alongside other inflammatory pathways could offer synergistic effects, improving symptom control in patients with severe and persistent eosinophilic diseases.
In conclusion, targeting PGD2 signaling through receptor antagonists and PGD2 synthesis inhibitors presents a promising therapeutic strategy for treating eosinophil-driven diseases. Continued research will help refine these treatments and broaden their applications to benefit a wider range of patients with allergic and non-allergic diseases.
References
- Heinemann, A., Sturm, E. M., & Peinhaupt, M. (2017). Prostaglandins and their receptors in eosinophil function and as therapeutic targets. Frontiers in Medicine, 4, 104. Link
- Peinhaupt, M., Sturm, E. M., & Heinemann, A. (2017). The prostanoid-eosinophil axis in allergic diseases. Frontiers in Medicine, 4, 104. Link
- Gervais, F. G., et al. (2001). Selective modulation of chemokinesis, degranulation, and apoptosis in eosinophils through the PGD2 receptors CRTH2 and DP. Journal of Allergy and Clinical Immunology, 108(6), 982-988. Link
- Bessa, C. J., et al. (2006). Eosinophils and their role in chronic inflammation. Journal of Leukocyte Biology, 80(6), 1231-1240. Link
- Shiraishi, Y., et al. (2005). Prostaglandin D2-induced eosinophilic airway inflammation is mediated by CRTH2 receptor. Journal of Pharmacology and Experimental Therapeutics, 312(3), 954–960. Link
- Fajt, M. L., et al. (2013). Prostaglandin D2 pathway upregulation: Relation to asthma severity, control, and TH2 inflammation. Journal of Allergy and Clinical Immunology, 131(6), 1504-1512. Link
- Steinke, J. W., et al. (2017). Aspirin-exacerbated respiratory disease: Pathophysiology and management strategies. Current Allergy and Asthma Reports, 17(2), 1-10. Link