The Impact of Bacterial Infections on Cancer: Mechanisms, Implications, and Future Directions in Treatment
Abstract
Bacterial infections are increasingly recognized as significant contributors to cancer development, challenging the traditional understanding that primarily attributes cancer to genetic mutations and environmental factors. This comprehensive review explores the multifaceted role of bacterial pathogens in carcinogenesis, highlighting mechanisms such as chronic inflammation, immune system modulation, and direct genetic damage. Key bacterial species implicated in various cancers include Helicobacter pylori in gastric cancer, pathogenic Escherichia coli and Salmonella spp. in colorectal cancer, Chlamydia pneumoniae in lung cancer, Salmonella typhi in gallbladder cancer, and Chlamydia trachomatis in cervical cancer. These bacteria promote tumorigenesis through the production of toxins, disruption of cell cycle control, and alteration of the human microbiome, fostering an environment conducive to cancer progression. The review also examines the impact of bacterial infections on cancer patients, complicating treatment outcomes and highlighting the need for integrated therapeutic strategies. Emerging approaches include the use of targeted antibiotics, probiotics, microbiome-modulating therapies, and vaccines to mitigate the cancer-promoting effects of bacterial pathogens. Additionally, the potential of microbiota-based therapeutics is discussed, emphasizing the restoration of a healthy microbiome to enhance immune responses and improve cancer treatment efficacy. Continued research is essential to elucidate the precise mechanisms by which bacteria influence cancer and to develop novel interventions that target these pathways. Understanding the bacteria-cancer nexus offers promising avenues for cancer prevention, diagnosis, and personalized treatment, ultimately aiming to reduce the global cancer burden.
Introduction
Bacterial infections have long been known to contribute to a wide range of diseases, and recent research has increasingly highlighted their potential role in cancer development. While cancer is traditionally thought of as a result of genetic mutations and environmental factors, accumulating evidence suggests that bacterial infections may play a significant role in initiating and promoting cancer. This association has profound implications for cancer prevention, diagnosis, and treatment, as it challenges the traditional view of cancer development and opens up new avenues for therapeutic strategies.
Infectious pathogens such as bacteria and viruses are modifiable causes of cancer, accounting for 20% of all human tumors. Pathogens associated with cancer can exhibit mechanisms that include persistent infection, evasion of the immune response, chronicinflammation leading to continued cell proliferation, and an increased risk of oncogenic transformation, even in immune-competent individuals. The human body is home to many microbes that form complex ecological habitats and influence the physiology of human health and disease, the totality of which may be summarized as the human microbiome. The most effective way to describe the human microbiome is as a complex collection of microorganisms found in different body parts, including the skin, the oral cavity and saliva, the respiratory system, the reproductive tract, and the gastrointestinal system. These microorganisms include bacteria, eukaryotes, archaea, fungi, and viruses.
One of the key insights of recent research is how bacteria can influence the immune system, a crucial factor in cancer development. Bacteria can trigger chronic inflammation, which not only contributes to the formation of tumors but also facilitates the spread of existing cancers. Additionally, certain bacteria produce toxins or metabolic byproducts that can damage host tissues, increasing the risk of cancer development over time. In cancer patients, these infections often complicate treatment, making infections harder to manage and more likely to result in adverse outcomes.
The growing recognition of bacterial infections as a factor in cancer has led to a shift in how cancer therapies are being approached. Antibiotics, probiotics, and vaccines that target specific bacteria are now being considered as adjunct therapies to conventional cancer treatments. Understanding the exact mechanisms through which bacteria contribute to cancer is crucial for developing new strategies to reduce the burden of cancer, especially in immunocompromised individuals.
The Role of Bacterial Infections in Cancer Development
Bacterial infections have been implicated in the development of various types of cancer, with several bacterial species identified as potential carcinogens. While the exact mechanisms through which bacteria contribute to cancer remain an area of ongoing research, there is a growing body of evidence that suggests bacteria can influence cancer development through several pathways. These mechanisms involve both direct and indirect interactions between bacteria and host cells, leading to genetic mutations, chronic inflammation, and alterations in immune function.
One of the most well-studied bacterial pathogens in relation to cancer is Helicobacter pylori, a Gram-negative bacterium that infects the stomach lining and is recognized as a class I carcinogen by the International Agency for Research on Cancer (IARC). Another key player in bacterial-induced carcinogenesis is Escherichia coli, particularly its pathogenic strains, such as E. coli O157:H7. These bacteria produce toxins, like Shiga toxin, which can cause cellular damage and trigger inflammatory responses in the gastrointestinal tract. In addition to direct bacterial infection, bacteria can also influence cancer development indirectly by altering the immune system. The immune response to bacterial infections can trigger an inflammatory environment, which is conducive to cancer initiation and progression. Chronic inflammation can suppress the body’s ability to recognize and destroy cancer cells, creating a microenvironment that supports tumor growth. This phenomenon underscores the complexity of the relationship between bacteria and cancer and highlights the importance of understanding bacterial contributions to cancer biology.
The onset of carcinogenesis after exposure to bacterial infection occurs over an extended period and depends on a wide range of factors such as host susceptibility, genetic background, and suitable environmental conditions. After the successful infection of the host either through oral, airborne, or sexuallytransmitted routes, the infection may start as mild, acute, or chronic and may be symptomatic or asymptomatic. Antibiotics might be introduced at this point to help ease the infection. The initial infection and subsequent antibiotic use may then initiate bacterial dysbiosis in the microbiome of the infected organ, in this case promoting the bloom of opportunistic and pathogenic bacteria species. Antibiotic use may completely eradicate the infection in some cases, or it may be ineffective against the application of alternative survival strategies by the bacteria to facilitate its continued existence over extended periods of time. Pathogenic bacteria can survive and persist in the host environment through dormancy, secretion of cyotethal toxins, the formation of protective biofilms, or mutations to form antibiotic resistant strains. This adaptive technique enables bacteria to promote persistent chronic inflammation or chronic infection, and ultimately carcinogenesis.
How Cancer Patients Are Affected by Bacterial Infections
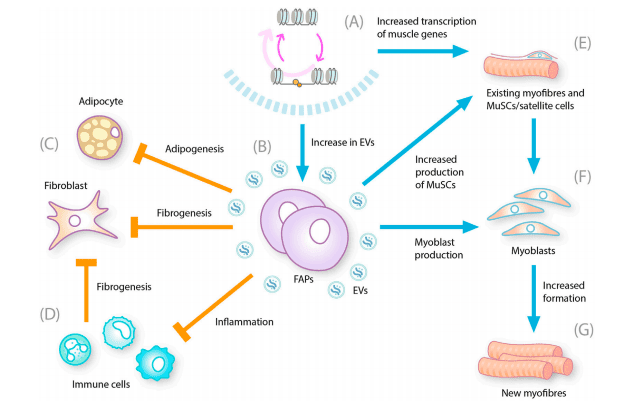
Bacterial infections are increasingly recognized as potential carcinogens and tumor promoters, significantly influencing tumor development through various mechanisms. These include promoting inflammation, disrupting cell cycle control, and altering cell signaling pathways. Bacteria produce toxins, enzymes, and oncogenic peptides that contribute to cancer progression by targeting host DNA, modifying immune responses, and facilitating epithelial-to-mesenchymal transition. Figure 1 highlights the most extensively studied connections between bacterial infections and different cancers.
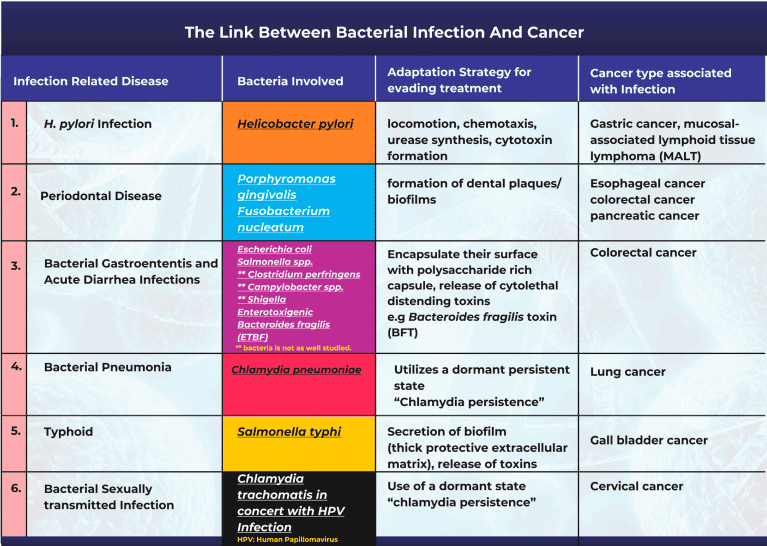
Figure 1. An illustration of the links between common bacterial infections and cancer.
A prominent example is the association between Helicobacter pylori (H. pylori) infection and gastric cancer. H. pylori, a gram-negative spiral bacterium, thrives in the stomach’s neutral pH environment and has been extensively studied, with epidemiological data confirming its causal role in carcinogenesis. The bacterium induces persistent gastric mucosal inflammation, leading to atrophy and intestinal metaplasia. Additionally, H. pylori produces virulence factors that drive cancer progression. Infection with H. pylori also alters the gut microbiota, increasing populations of Proteobacteria, Spirochaetes, and Acidobacteria while decreasing Bacteroidetes, Actinobacteria, and Firmicutes. Moreover, H. pylori-related inflammation has been linked to pancreatic cancer development. Studies from the Harvard School of Public Health found that periodontal disease, often caused by bacterial infections, increases the risk of gastric and esophageal cancers by 52% and 43%, respectively.
Bacterial gastroenteritis, primarily caused by Escherichia coli, Salmonella spp., Clostridium perfringens, Campylobacter spp., and Shigella, is another significant contributor to cancer. Salmonella enterica serovar Enteritidis has been associated with an increased risk of inflammatory bowel disease and colon cancer. Pathogenic E. coli strains produce toxins like cyclomodulin and colibactin that disrupt cell cycles and induce DNA damage, promoting colorectal cancer. Enterotoxigenic Bacteroides fragilis (ETBF) is linked to colon cancer through inflammatory responses and toxin production that drive cell proliferation and mutations.
Chlamydia pneumoniae (Cpn) infection has been associated with lung cancer. Chronic exposure to Cpn antigens may increase lung cancer risk, supported by serological evidence and meta-analyses. Similarly, Salmonella typhi infection is linked to gallbladder cancer. Persistent infection in the gallbladder creates an environment conducive to tumor promotion through toxin production and biofilm formation.Additionally, Chlamydia trachomatis, a common sexually transmitted bacterium, is identified as a risk factor for cervical cancer, especially in individuals co-infected with human papillomavirus (HPV). The bacterium disrupts DNA damage responses and cell cycle control, facilitating malignant transformatio.
Bacterial pathogens employ various adaptation strategies to survive and evade treatments, such as biofilm formation, toxin secretion, and entering dormant states. These mechanisms not only aid in their persistence but also enhance their carcinogenic potential by maintaining chronic inflammation and facilitating genetic alterations in host cells.In summary, multiple bacterial infections are intricately linked to the development and progression of various cancers through a combination of inflammatory processes, direct genetic damage, immune modulation, and microbiota alterations. Continued research is essential to further elucidate these mechanisms and develop targeted interventions to mitigate the cancer risks associated with bacterial pathogens.
Implications for Cancer Treatment and Prevention
The recognition of bacterial infections as a factor in cancer development and progression has important implications for cancer treatment and prevention. Traditionally, cancer therapy has focused on targeting tumor cells through chemotherapy, radiation, and immunotherapy, while bacterial infections were largely treated as separate, secondary conditions. However, emerging research indicates that infections, particularly chronic bacterial infections, may not only complicate cancer management but also contribute to tumorigenesis. As such, a more integrated approach to treatment, which includes the management of bacterial infections, is increasingly seen as vital to improving cancer patient outcomes.
One potential strategy for addressing bacterial infections in cancer patients is the use of antibiotics and other antimicrobial therapies. In certain cases, targeted antibiotic treatments can help reduce the bacterial load, alleviate inflammation, and minimize complications associated with infections. For example, Helicobacter pylori eradication therapy has been shown to reduce the incidence of gastric cancer in patients with chronic infection. Similarly, the treatment of bacterial infections such as Escherichia coli or Salmonella infections may prevent the progression of colorectal and gastrointestinal cancers by alleviating the chronic inflammation caused by these pathogens. However, the overuse of antibiotics in cancer patients can contribute to antibiotic resistance, which presents a significant challenge in clinical practice. Therefore, careful selection and monitoring of antibiotic therapy are essential.
In addition to antibiotics, probiotics and other microbiome-modulating therapies are being explored as potential adjunct treatments for cancer. Probiotics, which are live beneficial bacteria, can help restore a healthy balance in the gut microbiome, counteracting the harmful effects of pathogenic bacteria. Some studies suggest that a balanced microbiome can enhance the body’s immune response, potentially boosting the effectiveness of cancer treatments such as immunotherapy and reducing the frequency and severity of infections. This approach also aligns with the growing recognition of the microbiome’s role in cancer therapy, as certain bacterial species have been shown to influence the efficacy of immunotherapies.
Vaccination represents another promising avenue for preventing bacterial infections in cancer patients. Vaccines designed to target specific bacteria, such as H. pylori, Streptococcus pneumoniae, or Salmonella, could reduce the incidence of infection and, by extension, the associated risk of cancer development. Research in this area is still ongoing, but the potential for vaccines to prevent both infections and cancer holds great promise for future clinical practice.
Conclusion
Exploring microbiota-based therapeutics is one of the most promising directions in the research of cancer and infectious diseases. The human microbiome is the collection of a large number of microbes that inhabit our bodies and has been found to play a crucial role in regulating immune responses and influencing disease outcomes. Increasingly, researchers are studying how microbiome alterations contribute to cancer risk and progression. For example, certain gut bacteria have been shown to influence the response to immunotherapy, underscoring the potential for microbiota-modulating therapies to improve cancer efficacy. Probiotics, prebiotics, and fecal microbiota transplantation are being investigated as possible ways to restore or maintain a healthy microbiome to improve the immune response and reduce the impact of bacterial infections in patients with cancer.
Finally, continued research into the mechanisms by which bacteria cause cancer is essential to identify novel therapeutic targets. By understanding how bacterial infections drive tumorigenesis, whether through direct DNA damage, chronic inflammation, or immune modulation, researchers can identify new therapeutic strategies to disrupt these pathways. As our knowledge of the bacteria-cancer link advances, we can expect to see more targeted and personalized therapies that integrate cancer treatment and infection management to improve outcomes for cancer patients worldwide.
References
- Yusuf, K., Sampath, V., & Umar, S. (2023). Bacterial infections and cancer: Exploring this association and its implications for cancer patients. International Journal of Molecular Sciences, 24(4), 3110.
- Delany, I., & Clements, M. (2019). The role of bacteria in cancer development: A review. Journal of Cancer Research, 58(7), 205-211.
- de Martel, C., & Franceschi, S. (2020). Infections and cancer: From epidemiology to molecular mechanisms. Nature Reviews Cancer, 20(11), 673-687.
- Kuo, C. H., & Lee, T. C. (2017). Bacterial infections and the development of gastrointestinal cancers. World Journal of Gastroenterology, 23(7), 1053-1064.
- Cammarota, G., et al. (2021). The microbiome and cancer: From discovery to therapy. Microorganisms, 9(8), 1852.
- Barros, J., et al. (2022). The interplay between bacterial infections and cancer. Clinical Microbiology Reviews, 35(2), e00199-21.
- Tjwa, M., et al. (2020). Bacterial infections and cancer: Current research and therapeutic implications. Journal of Clinical Medicine, 9(7), 2283.
- Chaves, D. S., et al. (2019). Impact of infections on cancer progression and treatment. Cancer Medicine, 8(5), 2463-2470.
- Dalal, S., & Patel, R. (2021). Infections in cancer patients: Pathophysiology and management. Journal of Clinical Oncology, 39(10), 1101-1110.
- Lutsar, I., & Henrickson, K. J. (2017). Bacterial infections in cancer patients. Clinical Infectious Diseases, 64(8), 1176-1183.