Treprostinil: A Comprehensive Approach to Pulmonary Hypertension Management
Abstract
Pulmonary arterial hypertension (PAH) is a progressive disease characterized by elevated pulmonary vascular resistance leading to right heart failure with poor prognosis. Despite advances in medical therapy, the average life expectancy is 5 to 6 years. The prostacyclin analogue treprostinil has become a key treatment option for PAH. It significantly improves exercise capacity, clinical symptoms, and long-term survival. Treprostinil is administered subcutaneously, intravenously, or by inhalation and offers flexibility in dosing and delivery, making it a more convenient and stable alternative to epoprostenol. Recent advances in oral and inhaled formulations aim to improve adherence, while ongoing studies explore their efficacy in other forms of pulmonary hypertension, including chronic thromboembolic pulmonary hypertension (CTEPH). However, challenges such as optimizing dosing and managing side effects such as pain at the infusion site remain. Continued research is essential to refine the use of treprostinil and expand its therapeutic potential.
Introduction
Treprostinil is widely used to treat pulmonary arterial hypertension (PAH). PAH is a dyspnea-fatigue syndrome defined by an isolated increase in pulmonary vascular resistance (PVR) bringing about progressive right heart failure . In spite of significant advances achieved with the introduction of prostacyclins, endothelin receptor antagonists (ERA), and phosphodiesterase-5 (PDE-5) inhibitors , the prognosis of PAH remains unfavorable, with estimated medial life expectancies of 5–6 years, and insufficient clinical improvement in about half of the survivors after 1–2 years.PAH occurs in association with various conditions, which include connective tissue diseases (CTD), human immunodeficiency virus (HIV) infection, portal hypertension , congenital heart diseases (CHD), and intake of appetite-suppressant drugs, mainly fenfluramines.
n the early 1990s, pulmonary arterial hypertension (PAH) was considered a uniformly fatal disease with a median life expectancy of only 2.5 years. Initial studies indicated that a small percentage of patients responded to high-dose calcium channel blockers, while retrospective studies supported anticoagulant therapy. Conventional treatments were limited to lifestyle modifications, diuretics, digitalis, and supplemental oxygen. The introduction of chronic intravenous prostacyclin in the 1980s, specifically epoprostenol, marked a turning point, particularly for patients with idiopathic PAH (IPAH), bridging them to transplantation. Subsequent randomized controlled trials demonstrated that epoprostenol significantly improved functional status, exercise capacity, and survival in both IPAH and connective tissue disease-associated PAH (CTD-PAH). These findings led to FDA approval for its use in New York Heart Association (NYHA) functional classes III and IV IPAH patients in 1996, with a label extension for CTD-PAH in 2000. Long-term studies have shown sustained clinical benefits in various forms of PAH, including congenital heart disease (CHD), portal hypertension-associated PAH, and HIV-related PAH. Epoprostenol has even allowed some patients to be removed from transplantation waiting lists. While it remains the gold standard for PAH treatment, particularly for NYHA class IV patients, it is not without limitations.
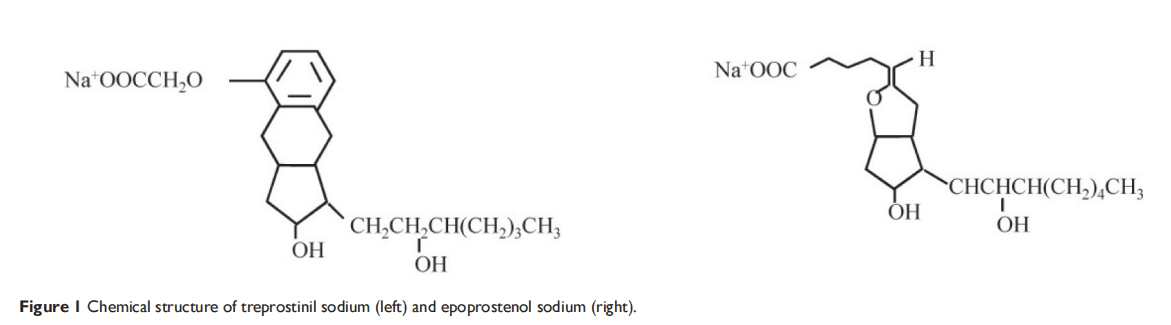
Due to its instability and short half-life (2–7 minutes), epoprostenol requires continuous infusion via a central venous catheter, leading to risks such as catheter-related embolism, thrombosis, infections, and delivery system malfunctions causing overdosing or under-dosing. To address these issues, more stable prostacyclin derivatives and alternative administration routes, such as subcutaneous treprostinil, were developed.
Pharmacology of Treprostinil
Treprostinil is a tricyclic benzindene analogue of prostacyclin, exhibiting similar anti-platelet and vasodilatory properties, including acute pulmonary vasodilation. After subcutaneous administration, treprostinil is rapidly and completely absorbed, with an absolute bioavailability of 100%. Continuous subcutaneous infusion leads to steady-state plasma concentrations within approximately 10 hours, with dosing rates ranging from 1.25 to 22 ng/kg/min. Treprostinil is primarily metabolized in the liver, though the specific enzymes involved remain unidentified. Around 79% of the administered dose is excreted via urine, with 4% as the unchanged drug and 64% as identifiable metabolites. Treprostinil has a favorable safety profile, showing no reproductive toxicity or teratogenic effects.
However, treprostinil clearance can decrease by up to 80% in patients with hepatic insufficiency, necessitating cautious dosing in patients with PAH linked to liver disease. Currently, there are no pharmacokinetic studies on treprostinil in patients with renal insufficiency. Importantly, treprostinil does not interfere with the metabolism of drugs like paracetamol, warfarin, or digoxin. Chemically, treprostinil remains stable in sterile water, 0.9% sodium chloride, or 5% dextrose solutions at room temperature, with a nearly neutral pH, ensuring its stability for clinical use.
Subcutaneous treprostinil offers significant advantages over intravenous epoprostenol due to its simpler delivery system and the elimination of the need for a surgically implanted central venous catheter. While epoprostenol requires sterile reconstitution once or twice daily, along with ice packing and the use of bulky portable pump systems, treprostinil is much more convenient. It is provided in 20 mL vials with concentrations of 1, 2.5, 5, or 10 mg/mL, which can be stored at room temperature. Treprostinil is administered through a compact mini-infusion pump, approximately the size of a small cell phone, making it much more portable. The injection site typically needs to be changed every three days. However, despite recommendations, many patients find it more comfortable to leave the subcutaneous catheter in place for up to 2–3 weeks, and this practice has generally been well tolerated.
Pharmacology and Mechanism of Action
Treprostinil is a prostacyclin analogue that provides vasodilatory and anti-platelet effects, making it highly effective in treating pulmonary hypertension (PH). As a tricyclic benzindene prostacyclin, treprostinil works by relaxing the blood vessels in the lungs, thereby reducing pulmonary vascular resistance and relieving the strain on the right side of the heart (Vachiery & Naeije, 2004). One of its key benefits is its stability and long half-life, which distinguishes it from other prostacyclin therapies. Treprostinil can be administered via subcutaneous, intravenous, and inhaled routes, allowing for flexibility in treatment based on patient needs and tolerability.
Subcutaneous administration, in particular, has gained popularity due to the absence of the risks associated with central venous catheters, such as infections and thrombosis, which are common with intravenous prostacyclin therapy. Treprostinil’s favorable pharmacokinetics include 100% bioavailability when administered subcutaneously, and it is primarily metabolized in the liver, with most of the drug excreted in urine.
The pivotal 12-week trial involved two parallel international, multicenter, double-blind, randomized, placebo-controlled studies conducted in North America and Europe. A total of 470 patients, aged 8 to 75 years, with pulmonary arterial hypertension (PAH) participated. This trial remains the largest randomized controlled study in PAH to date. The primary endpoint was the 6-minute walk distance, assessing exercise capacity. Additional endpoints included a dyspnea-fatigue rating and a clinical score based on symptoms such as dyspnea, orthopnea, chest pain, and dizziness. A simplified version of the clinical score, focusing on five symptoms, proved equally sensitive to treatment. Secondary endpoints included the Borg score and hemodynamic measurements such as right atrial pressure and cardiac output. Quality of life was measured using the Minnesota Living with Heart Failure questionnaire.
Treprostinil was administered at a starting dose of 1.25 ng/kg/min, gradually increased to a maximum of 22.5 ng/kg/min over 12 weeks, though the average dose achieved was lower due to infusion site pain. The treprostinil group’s median 6-minute walk distance increased by 10 meters, compared to no change in the placebo group, with a between-group difference of 16 meters (p = 0.0064). Though the studies did not individually reach statistical significance (p-values of 0.0607 and 0.055), the pooled analysis supported a treatment effect.
Subgroup analysis revealed significant interactions between treatment effects and factors such as NYHA class, baseline 6-minute walk distance, and SvO2. The highest improvement was observed in patients in NYHA class IV. The primary adverse effect in the treprostinil group was infusion site pain, leading to treatment discontinuation in 8% of patients. Other side effects included diarrhea, jaw pain, flushing, and lower limb edema.
Clinical Trials and Efficacy
The efficacy of treprostinil has been demonstrated in multiple clinical trials. A pivotal 12-week randomized, placebo-controlled study showed significant improvements in exercise capacity, measured by the 6-minute walk distance test, in patients treated with subcutaneous treprostinil . This trial also demonstrated improvements in clinical symptoms such as dyspnea, fatigue, and overall functional class.
Long-term studies have shown that the benefits of treprostinil extend beyond the initial treatment period. In a large observational study, treprostinil was associated with improved survival rates, with 87% of patients surviving at one year and 68% at four years. Treprostinil’s flexibility in dosing and modes of administration, combined with its effectiveness in improving clinical outcomes, have solidified its role as a key therapy in the management of PH.
Future Directions and Potential Applications of Treprostinil
Treprostinil can improve exercise capacity, clinical symptoms, and survival in patients with pulmonary arterial hypertension (PH), so it has become an integral part of the treatment of PH. In addition to its current application, the development of new formulations and potential uses of treprostinil signaling provides new directions for its treatment.
Inhaled treprostinil is a relatively new addition to the pulmonary vasodilator arsenal in pulmonary arterial hypertension.
Its efficacy for the treatment of PH-ILD, a subgroup previously without any proven PH-targeted treatment, is an exciting
new development. The introduction of a dry inhalation powder form of the drug presents an option for drug delivery that is less cumbersome and more convenient than the nebulized form with a similar profile of adverse effects. New forms of inhaled treprostinil powder are also in development and may further expand the ability to deliver the drug to both PAH and PH-ILD patients when they enter the greater market.
The role of treprostinil in the treatment of other forms of pulmonary hypertension, such as chronic thromboembolic pulmonary hypertension (CTEPH), is also being investigated. Small studies suggest that treprostinil may be beneficial in CTEPH, especially in patients who are not surgical candidates. In addition, preoperative administration of treprostinil in patients with high pulmonary vascular resistance has been suggested as a potential approach to improve surgical outcomes.
Despite the benefits, challenges remain, such as optimizing dosing and managing side effects such as pain at the infusion site. Continued research will help refine the application of treprostinil and provide new hope for patients with PH and related diseases.
References
- Cassady, S. J., Almario, J. A. N., & Ramani, G. V. (2024). Therapeutic potential of treprostinil inhalation powder for patients with pulmonary arterial hypertension: Evidence to date. Drug, Healthcare and Patient Safety, 16, 51-59.
- Nika Skoro-Sajer, Irene Lang & Robert Naeije (2008) Treprostinil for pulmonary hypertension, Vascular Health and Risk Management, 4:3, 507-513.
- Barst, R. J., Rubin, L. J., Long, W. A., McGoon, M. D., Rich, S., Badesch, D., … Groves, B. M. (1996). A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension. New England Journal of Medicine, 334(5), 296-301.
- Farber, H. W., & Loscalzo, J. (2004). Pulmonary arterial hypertension. New England Journal of Medicine, 351(16), 1655-1665.
- Humbert, M., Sitbon, O., Chaouat, A., Bertocchi, M., Habib, G., Gressin, V., … Simonneau, G. (2006). Pulmonary arterial hypertension in France: Results from a national registry. American Journal of Respiratory and Critical Care Medicine, 173(9), 1023-1030.
- Vachiery, J. L., & Naeije, R. (2004). Treprostinil for pulmonary hypertension. Expert Review of Cardiovascular Therapy, 2(2), 183-191.
- Wade, M., Baker, F. J., Roscigno, R., Weiser, W. E., & Hunt, T. L. (2003). Effect of continuous subcutaneous treprostinil therapy on the pharmacodynamics and pharmacokinetics of warfarin. Journal of Cardiovascular Pharmacology, 41(6), 908-915.
- Channick, R. N., Olschewski, H., Seeger, W., Staub, T., Rubin, L. J., & Speich, R. (2006). Safety and efficacy of inhaled treprostinil as add-on therapy to bosentan in pulmonary arterial hypertension. Journal of the American College of Cardiology, 48(7), 1433-1437.




