Understanding Epilepsy: Causes, Symptoms, and Latest Treatment Approaches
Abstract
Epilepsy is a chronic neurological disorder characterized by recurrent, unprovoked seizures, affecting millions globally. Research into its causes, mechanisms, and treatment options has significantly advanced, especially in areas like genetics, personalized medicine, and novel therapeutic interventions. This article explores recent breakthroughs in epilepsy research, including the identification of genetic mutations, advancements in neuroimaging, and the development of new treatments such as responsive neurostimulation (RNS), neuromodulation therapies, and gene editing. Additionally, emerging therapies like cannabinoid-based treatments and mTOR inhibitors are being investigated for their potential in treating drug-resistant epilepsy. The article also discusses the role of precision medicine and biomarker discovery in developing targeted, individualized therapies. As research continues, these innovations promise to offer more effective treatments, improve patient outcomes, and deepen our understanding of the complex biological processes underlying epilepsy.
Introduction
Epilepsy is a chronic neurological disorder that affects the brain’s electrical activity, leading to recurrent, unprovoked seizures. These seizures occur when abnormal electrical discharges in the brain cause temporary disruptions in normal brain function. Epilepsy is one of the most common neurological conditions, affecting approximately 50 million people worldwide, across all ages and ethnicities. It can develop at any stage of life and has a wide range of manifestations, from mild, brief episodes to severe, prolonged seizures that impair consciousness and motor functions.
The importance of raising awareness and understanding epilepsy in medical research and treatment cannot be overstated. Although epilepsy is treatable, many individuals continue to experience uncontrolled seizures, particularly those who have drug-resistant epilepsy. Increased awareness helps reduce the stigma surrounding the condition and encourages better diagnosis and management. Research into the causes of epilepsy, its various types, and personalized treatment approaches is essential for advancing care. Improved understanding of the genetic and environmental factors contributing to epilepsy has opened doors for new therapeutic options, including personalized medicine. By enhancing public and medical knowledge, we can foster better outcomes for patients, improve quality of life, and reduce the global burden of epilepsy.
What is Epilepsy?
Definition of Epilepsy
Epilepsy is a chronic neurological disorder characterized by recurrent, unprovoked seizures caused by abnormal electrical activity in the brain. Seizures are sudden bursts of electrical discharges in brain cells that disrupt normal brain function. The severity and type of seizures can vary widely, ranging from brief lapses in awareness to full-body convulsions. Epilepsy is diagnosed when a person experiences two or more unprovoked seizures more than 24 hours apart.
Prevalence and Types of Epilepsy
Epilepsy affects approximately 50 million people worldwide, making it one of the most common neurological disorders. It affects individuals of all ages, but it is most often diagnosed in childhood or in older adults. There are two broad categories of epilepsy: focal epilepsy and generalized epilepsy. Focal epilepsy involves seizures that start in one part of the brain, while generalized epilepsy affects both sides of the brain. Specific types of seizures, such as tonic-clonic seizures, absence seizures, and focal seizures, are classified based on their symptoms and the areas of the brain involved.
The Neurological Mechanisms Behind Seizures
Seizures occur when the brain’s normal electrical signaling becomes disrupted. Neurons in the brain communicate through electrical impulses, and under normal conditions, this activity is balanced. In epilepsy, however, there is an imbalance in this electrical activity, either due to over-excitation or insufficient inhibition. This imbalance can be caused by genetic factors, brain injuries, infections, or other neurological conditions. When the electrical activity spreads abnormally, it leads to seizures, which can affect various brain functions, including movement, sensation, and consciousness.
Causes and Risk Factors of Epilepsy
Genetic Factors
Genetics can play a significant role in the development of epilepsy. Some individuals inherit genes that make them more susceptible to seizures, and certain genetic mutations are associated with specific types of epilepsy. These inherited factors can affect how the brain’s neurons respond to electrical signals, leading to abnormal brain activity. In many cases, genetic epilepsy syndromes are diagnosed in childhood, but some genetic factors may not manifest until later in life. Research has identified multiple genes involved in epilepsy, providing insights into its hereditary nature and offering potential targets for genetic therapies.
Brain Injuries and Trauma
Traumatic brain injuries (TBI) are a common cause of epilepsy, particularly in individuals who have experienced accidents, falls, or blunt force trauma to the head. Brain injuries can lead to scarring, changes in brain structure, or alterations in the brain’s electrical network, all of which can trigger seizures. Post-traumatic epilepsy (PTE) can occur immediately after a head injury or may develop months or even years later. The severity and location of the injury often influence the risk of developing epilepsy.
Infections and Stroke-Related Causes
Infections that affect the brain, such as meningitis, encephalitis, or brain abscesses, can cause lasting damage to brain tissue and lead to epilepsy. Infections can create inflammation and disrupt normal brain activity, increasing the likelihood of seizures. Similarly, stroke-related epilepsy can occur after a stroke disrupts the brain’s blood supply, leading to brain cell damage. The location and extent of the stroke can impact the development of epilepsy, with some individuals experiencing seizures shortly after the event.
Other Environmental Factors
Several environmental factors may increase the risk of developing epilepsy. Age is an important factor, as epilepsy is most commonly diagnosed in young children and older adults. Family history also plays a role, as individuals with a first-degree relative who has epilepsy are at a higher risk of developing the disorder themselves. Other environmental triggers, such as alcohol or drug abuse, sleep deprivation, or exposure to certain toxins, can also provoke seizures in susceptible individuals. Additionally, metabolic disorders, hormonal imbalances, or an imbalance in the brain’s neurotransmitters can contribute to the onset of epilepsy.

Fig.1 Causes of Epilepsy
Symptoms and Diagnosis
Common Symptoms of Epilepsy
The hallmark symptom of epilepsy is the occurrence of seizures, which vary widely in type and severity. Seizures are the result of abnormal electrical activity in the brain, and their manifestations depend on the area of the brain involved. Focal seizures, which start in one area of the brain, can cause symptoms such as twitching, unusual sensations, or a feeling of déjà vu. Generalized seizures, which affect both sides of the brain, can cause loss of consciousness and muscle jerking, as seen in tonic-clonic seizures (previously known as grand mal seizures). Other types of generalized seizures, such as absence seizures, can result in brief lapses in consciousness, often without any noticeable movements.
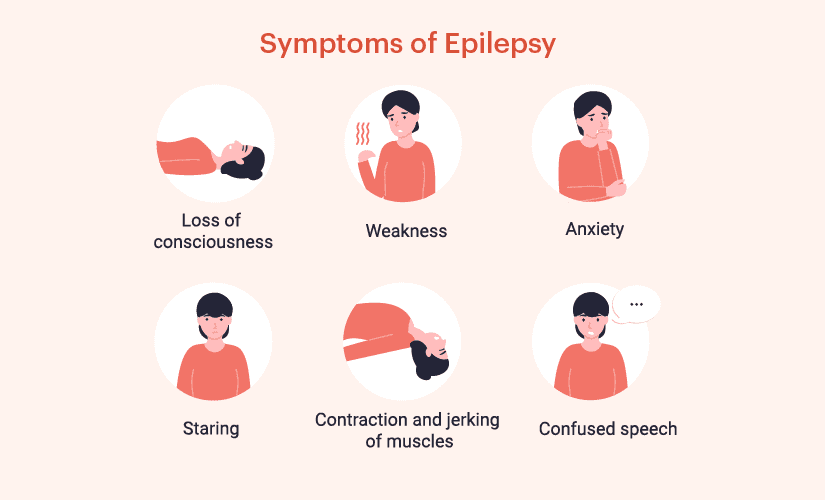
Fig. 2 Symptom of Epilepsy
In some cases, individuals experience an aura before a seizure, which serves as a warning sign. The aura is a type of partial seizure that can manifest as unusual smells, tastes, or visual disturbances. Auras are often experienced as a sensation of deja vu or an intense feeling of fear or anxiety. These pre-seizure symptoms provide individuals with an opportunity to seek safety before the full seizure occurs.
Loss of consciousness is another common symptom, especially in generalized seizures. This can result in a person falling or injuring themselves during a seizure episode, further emphasizing the importance of seizure management and safety measures.
Diagnostic Procedures
Accurate diagnosis of epilepsy involves a combination of patient history, clinical evaluation, and specialized diagnostic tests. One of the most important diagnostic tools is electroencephalography (EEG), which records the brain’s electrical activity. During an EEG, small electrodes placed on the scalp detect the electrical signals in the brain, allowing doctors to identify abnormal patterns of activity associated with seizures.
Magnetic resonance imaging (MRI) and computed tomography (CT) scans are also crucial in diagnosing epilepsy. MRI provides detailed images of the brain’s structure, helping to identify any abnormalities such as tumors, scar tissue, or malformations that could be causing seizures. CT scans are useful in emergency settings to detect any structural issues like bleeding or swelling in the brain.
Differentiating Between Different Types of Seizures
Distinguishing between different types of seizures is essential for accurate diagnosis and appropriate treatment. Seizures are categorized into focal and generalized types, but within these categories, there are various subtypes. For example, focal seizures may be further classified into simple partial seizures (where the person remains conscious) and complex partial seizures (where consciousness is impaired). Generalized seizures, which affect both sides of the brain, include tonic-clonic seizures, absence seizures, and myoclonic seizures (which cause brief muscle jerks).
The characteristics of a person’s seizure, including onset, duration, and specific movements or behaviors, provide critical information for classification. Additionally, EEG patterns often play a crucial role in determining the seizure type and localizing the brain area involved. Accurate classification of seizure types is necessary for choosing the most effective treatment plan for the patient.
Treatment Options for Epilepsy
Anti-Epileptic Drugs (AEDs) and Their Mechanisms
Anti-epileptic drugs (AEDs) are the cornerstone of epilepsy treatment, helping to control seizures in the majority of patients. AEDs work by altering the electrical activity in the brain to prevent the abnormal neuronal firing that leads to seizures. Different classes of AEDs target various mechanisms within the brain. Some, like sodium channel blockers (e.g., phenytoin, carbamazepine), work by stabilizing the neuronal membrane and preventing the rapid firing of neurons. GABAergic drugs (e.g., valproate, benzodiazepines) increase the inhibitory effects of gamma-aminobutyric acid (GABA), a neurotransmitter that reduces neuronal excitability. Other AEDs, like calcium channel blockers (e.g., ethosuximide), block the influx of calcium ions into neurons, reducing excitability. Despite the efficacy of AEDs, around one-third of patients with epilepsy experience drug-resistant seizures, requiring alternative treatments.
Surgical Options and Device Implantation
For patients with drug-resistant epilepsy, surgery may offer a potential cure. Resective surgery involves removing the brain tissue where seizures originate. This is most effective for focal seizures localized to a specific brain area. Laser ablation is a less invasive alternative, using focused laser beams to target and destroy the seizure-causing tissue. In cases where surgery is not an option, device implantation may be considered. Vagus Nerve Stimulation (VNS) involves implanting a device under the skin that sends electrical pulses to the vagus nerve, which in turn modulates brain activity and reduces seizure frequency. Another device, responsive neurostimulation (RNS), involves implanting a small device in the skull that detects abnormal brain activity and delivers electrical stimulation to prevent seizures.
Emerging Treatments
Advances in medical research have introduced several promising treatments for epilepsy, particularly for patients who do not respond to traditional therapies. Gene therapy is an emerging approach that aims to correct genetic mutations responsible for some types of epilepsy, potentially offering long-term solutions for genetic epilepsy syndromes. Medical cannabis has garnered attention for its anticonvulsant properties, particularly cannabidiol (CBD), which has been shown to reduce seizure frequency in certain types of epilepsy, such as Dravet syndrome and Lennox-Gastaut syndrome. The growing body of evidence supports its use, although more research is needed to establish standardized dosing and long-term safety. Additionally, dietary therapies such as the ketogenic diet, a high-fat, low-carbohydrate diet, have been found effective in reducing seizures in some patients, especially children with drug-resistant epilepsy.
Ongoing Research and Future Directions
Recent Advancements in Epilepsy Research
Epilepsy research has made significant strides in recent years, particularly in understanding the underlying genetic and molecular mechanisms of the disorder. Advances in genomics have allowed researchers to identify specific genes linked to different forms of epilepsy, leading to a deeper understanding of how genetic mutations disrupt brain activity and trigger seizures. Additionally, the advent of epigenetics has opened new avenues for exploring how environmental factors, such as diet, stress, and exposure to toxins, can influence gene expression and contribute to epilepsy. The use of advanced imaging techniques like functional MRI (fMRI) and magnetoencephalography (MEG) has also provided valuable insights into brain function and seizure localization, allowing for more precise diagnosis and targeted treatments.
Role of New Therapies and Technologies
Technological innovations are playing a key role in the development of new therapies for epilepsy. One such innovation is responsive neurostimulation (RNS), a device implanted in the brain that detects and responds to abnormal electrical activity by delivering targeted electrical pulses to prevent seizures. Similarly, neuromodulation techniques, including transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS), are being explored for their potential to modulate brain activity and reduce seizure frequency without the need for invasive procedures. Furthermore, genetic therapies and gene editing tools like CRISPR-Cas9 are being investigated for their potential to correct the genetic mutations responsible for certain types of epilepsy, potentially offering a long-term solution for patients with genetic forms of the disorder.
Potential Breakthroughs in Treatment and Understanding of Epilepsy
The future of epilepsy treatment lies in more personalized, targeted approaches. As we better understand the genetic and molecular mechanisms of epilepsy, the hope is to develop precision medicine tailored to the individual characteristics of each patient, such as their genetic makeup and the specific type of epilepsy they have. Biomarker discovery is an exciting area of research, as identifying specific biomarkers associated with epilepsy could lead to more accurate diagnosis and better monitoring of treatment efficacy.
Moreover, novel drug development is underway, with researchers exploring drugs that target previously unaddressed mechanisms in the brain. For example, mTOR inhibitors are being studied for their potential to treat epilepsy linked to tuberous sclerosis complex (TSC), a genetic disorder that causes tumor growth in the brain and leads to seizures. Another promising area is cannabinoid-based therapies, particularly cannabidiol (CBD), which has shown promise in clinical trials for treatment-resistant epilepsy.
As these innovations continue to unfold, breakthroughs in the understanding of epilepsy’s complex biology, along with the development of new therapies, offer hope for more effective treatments, better seizure control, and improved quality of life for those living with epilepsy.
References
Myers KA. Genetic Epilepsy Syndromes. Continuum (Minneap Minn). 2022 Apr 1;28(2):339-362. doi: 10.1212/CON.0000000000001077. PMID: 35393962.
https://pubmed.ncbi.nlm.nih.gov/35393962/
Katyayan A, Diaz-Medina G. Epilepsy: Epileptic Syndromes and Treatment. Neurol Clin. 2021 Aug;39(3):779-795. doi: 10.1016/j.ncl.2021.04.002. PMID: 34215386.
https://pubmed.ncbi.nlm.nih.gov/34215386/
Neri S, Mastroianni G, Gardella E, Aguglia U, Rubboli G. Epilepsy in neurodegenerative diseases. Epileptic Disord. 2022 Apr 1;24(2):249-273. doi: 10.1684/epd.2021.1406. PMID: 35596580.
https://pubmed.ncbi.nlm.nih.gov/35596580/
Pong AW, Xu KJ, Klein P. Recent advances in pharmacotherapy for epilepsy. Curr Opin Neurol. 2023 Apr 1;36(2):77-85. doi: 10.1097/WCO.0000000000001144. Epub 2023 Feb 10. PMID: 36762638.
https://pubmed.ncbi.nlm.nih.gov/36762638/
Golub V, Reddy DS. Cannabidiol Therapy for Refractory Epilepsy and Seizure Disorders. Adv Exp Med Biol. 2021;1264:93-110. doi: 10.1007/978-3-030-57369-0_7. PMID: 33332006.
https://pubmed.ncbi.nlm.nih.gov/33332006/
Fawcett J, Davis S, Manford M. Further advances in epilepsy. J Neurol. 2023 Nov;270(11):5655-5670. doi: 10.1007/s00415-023-11860-6. Epub 2023 Jul 17. PMID: 37458794.
https://pubmed.ncbi.nlm.nih.gov/37458794/




