Unlocking the Potential of TRPV4 Inhibition: A Promising Approach for Treating Lung Diseases
Abstract
This blog post explores the emerging therapeutic potential of inhibiting Transient Receptor Potential Vanilloid-4 (TRPV4) channels in the treatment of lung diseases. TRPV4 channels play crucial roles in maintaining respiratory homeostasis but are implicated in the pathogenesis of several severe respiratory conditions, including pulmonary hypertension, asthma, cystic fibrosis, and chronic obstructive pulmonary disease (COPD). By inhibiting TRPV4, it is possible to target the underlying mechanisms driving these diseases, offering new hope for more effective treatments. The post highlights recent research findings, the benefits of TRPV4 inhibition, promising TRPV4 inhibitors, and future research directions. This approach represents a significant advancement in lung disease treatment, potentially improving patient outcomes and quality of life.
Introduction
Lung diseases represent a significant global health burden, affecting millions of people worldwide. Conditions such as pulmonary hypertension, asthma, cystic fibrosis, and chronic obstructive pulmonary disease (COPD) lead to severe respiratory distress, reduced quality of life, and high mortality rates. Traditional treatments often focus on symptom management rather than addressing the underlying causes of these diseases. However, recent research has identified the transient receptor potential vanilloid-4 (TRPV4) channel as a promising therapeutic target for developing novel lung disease treatments.
TRPV4 channels are ion channels that play a critical role in various physiological processes, including the regulation of pulmonary blood flow, maintenance of fluid balance, and modulation of immune responses in lung tissues. These channels respond to a variety of stimuli, such as mechanical stress, temperature changes, and specific lipid mediators. Their widespread presence in lung tissues makes them a crucial component in maintaining respiratory homeostasis.
Research has shown that TRPV4 channels are upregulated in several life-threatening respiratory conditions. This upregulation is associated with increased disease severity and progression, making TRPV4 a potential target for therapeutic intervention. By inhibiting TRPV4 channels, it is possible to reduce the pathological processes that contribute to lung diseases. For instance, TRPV4 inhibition can prevent the abnormal vascular remodeling seen in pulmonary hypertension, reduce fluid leakage and edema in lung tissues, and mitigate inflammatory responses in conditions like asthma and COPD.
In summary, TRPV4 inhibition offers a promising new approach for treating various lung diseases. Targeting these channels could lead to the development of more effective therapies that address the root causes of respiratory conditions, ultimately improving patient outcomes and quality of life.
What are TRPV4 Channels?
Transient receptor potential vanilloid-4 (TRPV4) channels are a type of ion channel that play a critical role in various physiological processes within the body. These channels are part of the larger transient receptor potential (TRP) channel family, which is known for its involvement in sensing environmental changes and mediating cellular responses to different stimuli.
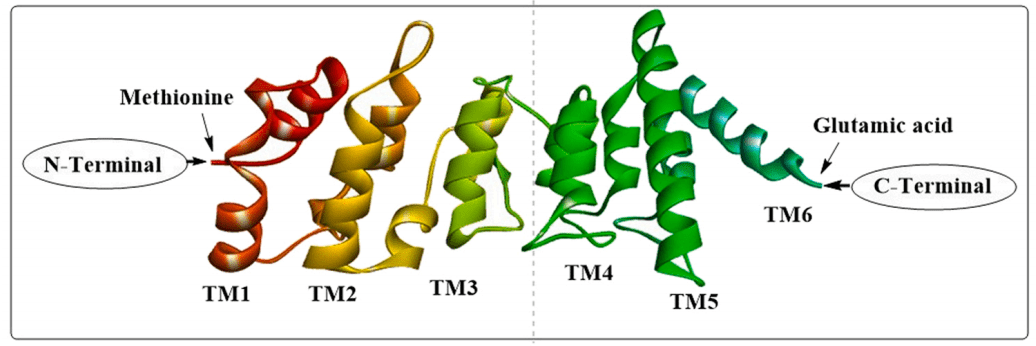
TRPV4 channels are permeable to calcium ions (Ca2+), and their activation leads to an influx of calcium into cells, triggering a cascade of intracellular events. These channels can be activated by a variety of stimuli, including mechanical stress (such as cell swelling or changes in osmolarity), temperature fluctuations, and certain chemical ligands like lipid mediators. This broad range of activation mechanisms allows TRPV4 to participate in diverse cellular functions.
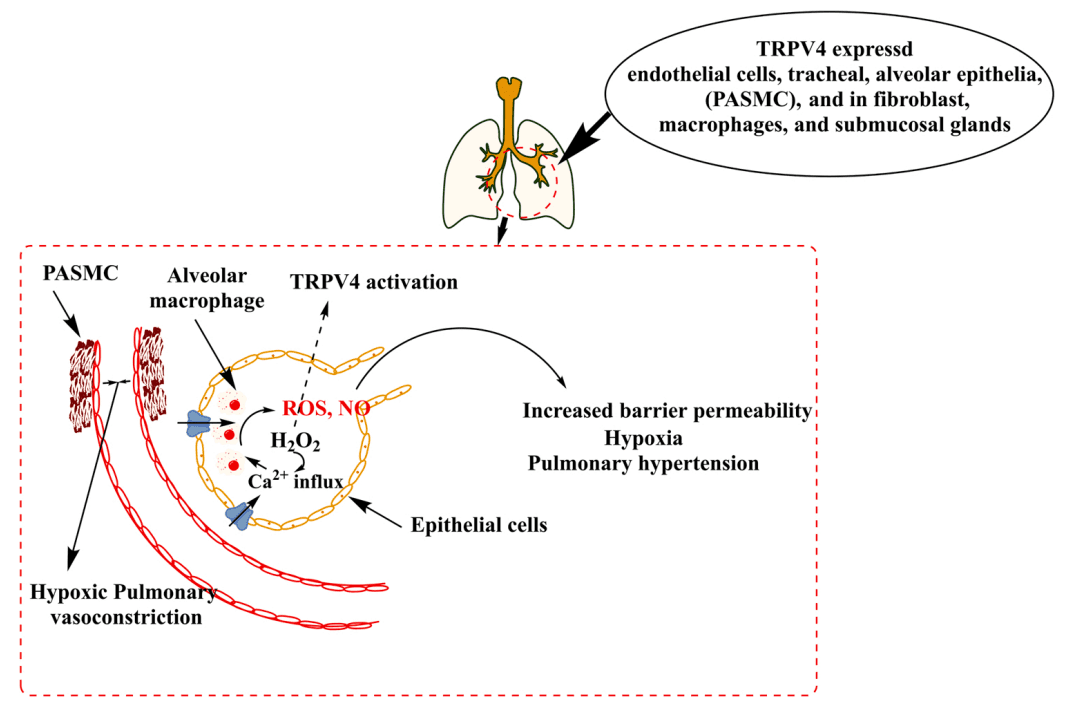
In the context of the respiratory system, TRPV4 channels are prominently expressed in several key areas of lung tissue. They are found in the pulmonary artery smooth muscle cells, vascular endothelium, airway epithelial cells, and the cilia of bronchial epithelial cells. Their strategic presence in these locations underscores their importance in maintaining respiratory homeostasis. For example, in pulmonary artery smooth muscle cells, TRPV4 channels help regulate pulmonary blood flow and vascular tone, which are essential for proper lung function and gas exchange.
Moreover, TRPV4 channels contribute to the maintenance of fluid homeostasis in the lungs by regulating the movement of ions and water across epithelial and endothelial barriers. This function is particularly important in preventing conditions such as pulmonary edema, where excessive fluid accumulates in the lung tissues. Additionally, TRPV4 channels play a role in modulating the immune response and inflammation within the respiratory system, further highlighting their significance in maintaining overall lung health.
The Role of TRPV4 in Lung Diseases
Transient receptor potential vanilloid-4 (TRPV4) channels play a significant role in various lung diseases. Their involvement in key physiological processes makes them critical in the pathogenesis and progression of several respiratory conditions, including pulmonary hypertension, asthma, cystic fibrosis, and chronic obstructive pulmonary disease (COPD).
Pulmonary Hypertension
Pulmonary hypertension is a severe lung disease characterized by increased blood pressure within the pulmonary arteries, leading to right heart failure. TRPV4 channels are upregulated in pulmonary hypertension, contributing to the disease by mediating calcium influx into pulmonary artery smooth muscle cells. This calcium influx leads to vasoconstriction and vascular remodeling, exacerbating the high blood pressure in the lungs. Inhibition of TRPV4 can help reduce these pathological changes, offering a potential therapeutic strategy for managing pulmonary hypertension.
Asthma
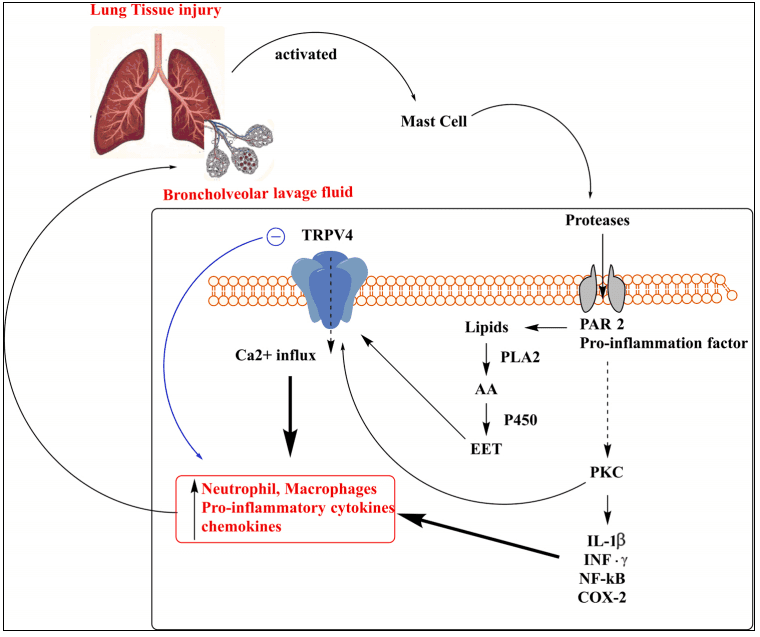
Asthma is a chronic inflammatory disease of the airways, marked by airway hyperresponsiveness, excessive mucus production, and episodic bronchoconstriction. TRPV4 channels contribute to asthma pathophysiology by modulating inflammatory responses and enhancing airway sensitivity to allergens. Activation of TRPV4 leads to the release of pro-inflammatory cytokines and increased mucus secretion, worsening asthma symptoms. Targeting TRPV4 can potentially reduce inflammation and improve airway function in asthma patients.
Cystic Fibrosis
Cystic fibrosis is an inherited disorder that affects the lungs and digestive system, characterized by thick, sticky mucus production that can clog airways. TRPV4 channels are implicated in cystic fibrosis through their role in regulating ion transport and mucus production in the airways. Defective TRPV4 function leads to impaired calcium signaling and mucus clearance, contributing to the disease’s severity. Enhancing or restoring TRPV4 function may help improve mucus clearance and reduce lung infections in cystic fibrosis patients.
Chronic Obstructive Pulmonary Disease (COPD)
COPD is a progressive lung disease characterized by chronic inflammation, airway obstruction, and alveolar destruction. TRPV4 channels are involved in COPD by mediating inflammatory responses and contributing to airway remodeling. Increased TRPV4 activity leads to elevated levels of inflammatory mediators and promotes structural changes in the airways, exacerbating COPD symptoms. Inhibiting TRPV4 can help mitigate inflammation and prevent further airway damage in COPD patients.
In summary, TRPV4 channels are crucial in the development and progression of various lung diseases. By understanding the mechanisms through which TRPV4 contributes to these conditions, researchers can develop targeted therapies that inhibit TRPV4 activity, offering new hope for patients with pulmonary hypertension, asthma, cystic fibrosis, and COPD.
Key Findings from Recent Research
Recent studies have highlighted the critical role of TRPV4 channels in the pathophysiology of various lung diseases. The key findings emphasize TRPV4’s involvement in pulmonary hypertension, lung edema, lung fibrosis, and chronic lung injury.
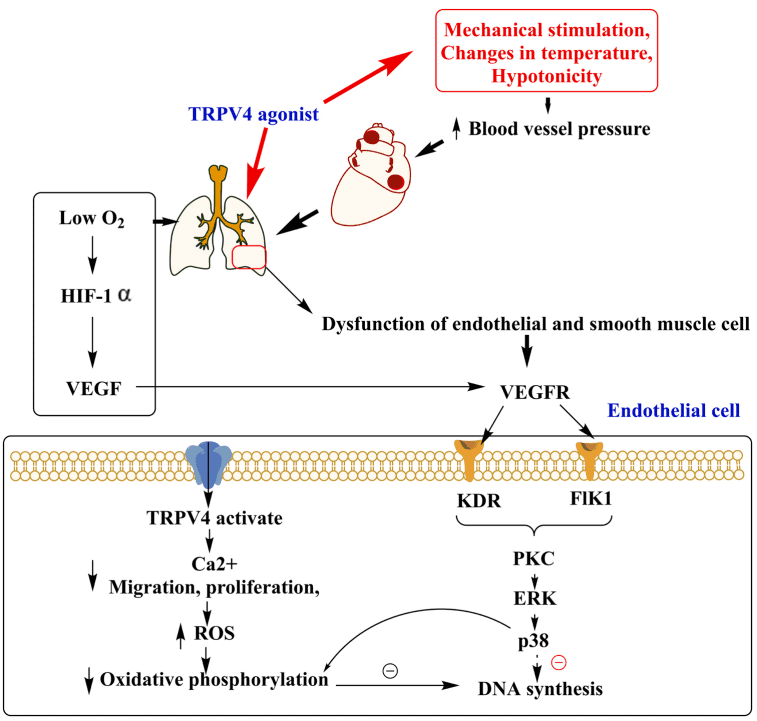
TRPV4’s Role in Pulmonary Hypertension and Vascular Remodeling
Research has shown that TRPV4 channels contribute significantly to pulmonary hypertension by mediating calcium influx into pulmonary artery smooth muscle cells. This calcium influx promotes vasoconstriction and vascular remodeling, exacerbating the high blood pressure in the lungs. Inhibiting TRPV4 has been demonstrated to reduce these pathological changes, offering a potential therapeutic strategy for managing pulmonary hypertension.
Contribution to Lung Edema and Increased Permeability
TRPV4 activation in endothelial cells increases vascular permeability, leading to fluid leakage and lung edema. This is particularly problematic in acute lung injury and chronic conditions such as heart failure. By inhibiting TRPV4, it is possible to decrease endothelial permeability and prevent fluid accumulation, thus mitigating lung edema and improving respiratory function.
Implications in Lung Fibrosis and Chronic Lung Injury
TRPV4 channels are also implicated in lung fibrosis, a condition characterized by excessive tissue scarring and impaired lung function. TRPV4-mediated calcium signaling promotes the activation and proliferation of fibroblasts, contributing to the fibrotic process. Targeting TRPV4 can help inhibit these processes and potentially reverse or slow down the progression of lung fibrosis. Additionally, TRPV4 inhibition has shown protective effects in various models of chronic lung injury, highlighting its therapeutic potential.
These findings underscore the importance of TRPV4 as a target for developing new treatments for lung diseases. By addressing the underlying mechanisms of these conditions, TRPV4 inhibitors offer a promising avenue for more effective therapies.
Promising TRPV4 Inhibitors
Several TRPV4 inhibitors have shown promise in preclinical and clinical studies. These compounds offer new hope for treating lung diseases by specifically targeting and inhibiting TRPV4 activity.
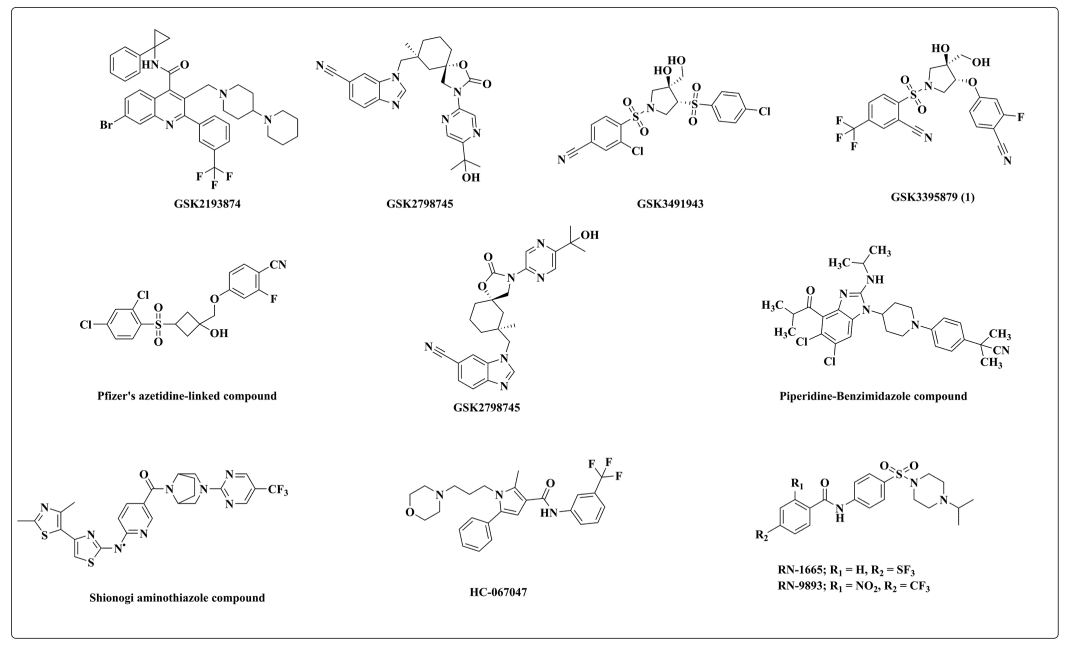
GSK2193874
GSK2193874 is a potent TRPV4 inhibitor that has demonstrated efficacy in reducing pulmonary edema and inflammation in animal models. It works by blocking the TRPV4-mediated calcium influx that leads to increased vascular permeability and fluid leakage. This inhibitor shows potential for treating conditions like pulmonary hypertension and heart failure-related lung edema.
RN-1734
RN-1734 is another selective TRPV4 antagonist that has shown promise in preclinical studies. It effectively blocks TRPV4 activation and prevents the pathological calcium signaling associated with various lung diseases. RN-1734 has potential applications in treating pulmonary hypertension, asthma, and COPD by reducing inflammation and improving airway function.
HC-067047
HC-067047 is a highly selective TRPV4 inhibitor that has been extensively studied for its therapeutic potential. It has shown efficacy in reducing lung edema, fibrosis, and injury in various experimental models. HC-067047 works by inhibiting TRPV4-mediated calcium influx, thus protecting against endothelial permeability and tissue remodeling. This inhibitor holds promise for treating a wide range of lung diseases, including pulmonary hypertension, lung fibrosis, and chronic lung injury.
In summary, the development of TRPV4 inhibitors like GSK2193874, RN-1734, and HC-067047 represents a significant advancement in the treatment of lung diseases. These compounds offer targeted therapeutic options that address the underlying mechanisms of these conditions, potentially improving patient outcomes and quality of life.
Future Directions and Research
Despite significant progress in understanding TRPV4 channels and their role in lung diseases, several gaps remain in the current research. Future studies are needed to elucidate the precise molecular mechanisms through which TRPV4 channels contribute to the pathogenesis of various lung conditions. Identifying these mechanisms will be crucial for developing highly specific and effective TRPV4 inhibitors.
Current Gaps in TRPV4 Research
One major gap in TRPV4 research is the limited understanding of the long-term effects of TRPV4 inhibition. While preclinical studies have shown promising results, the potential side effects and long-term safety of TRPV4 inhibitors need thorough investigation. Additionally, there is a need for more research on the interactions between TRPV4 channels and other signaling pathways involved in lung diseases.
Future Research Directions
Future research should focus on conducting comprehensive clinical trials to evaluate the efficacy and safety of TRPV4 inhibitors in humans. These trials should include diverse patient populations to understand better how different individuals respond to TRPV4-targeted therapies. Moreover, studies exploring combination therapies involving TRPV4 inhibitors and existing treatments could provide insights into more effective treatment regimens.
Potential Impact on the Treatment of Lung Diseases
The ongoing research into TRPV4 channels holds great promise for revolutionizing the treatment of lung diseases. By developing targeted therapies that inhibit TRPV4 activity, it is possible to address the underlying causes of conditions like pulmonary hypertension, asthma, cystic fibrosis, and COPD. Such advancements could lead to more effective treatments with fewer side effects, ultimately improving patient outcomes and quality of life.
Conclusion
In conclusion, TRPV4 inhibition represents a promising new approach for treating various lung diseases. The targeted nature of TRPV4 inhibitors allows for addressing the specific mechanisms driving disease progression, offering potential for more effective and sustained therapeutic outcomes.
As research continues to advance, staying updated with the latest findings is crucial for both medical professionals and patients. The development of TRPV4-targeted therapies could significantly improve the management of lung diseases, providing new hope for individuals affected by these debilitating conditions.
Reference
- Kumar, M., Zaman, M. K., Das, S., Goyary, D., Pathak, M. P., & Chattopadhyay, P. (2023). Transient Receptor Potential Vanilloid (TRPV4) channel inhibition: A novel promising approach for the treatment of lung diseases. Biomedicine & Pharmacotherapy, 163, 114861.
- Arniges, M., Vázquez, E., Fernández-Fernández, J. M., & Valverde, M. A. (2004). Swelling-activated Ca2+ entry via TRPV4 channel is defective in cystic fibrosis airway epithelia. Journal of Biological Chemistry, 279(52), 54062-54068.
- Dunham-Snary, K. J., Wu, D., Sykes, E. A., Thakrar, A., Parlow, L. R., Mewburn, J. D., … & Archer, S. L. (2017). Hypoxic pulmonary vasoconstriction: from molecular mechanisms to medicine. Chest, 151(1), 181-192.
- Brooks, C. A., Barton, L. S., Behm, D. J., Brnardic, E. J., Costell, M. H., Holt, D. A., … & Lawhorn, B. G. (2019). Discovery of GSK3527497: A candidate for the inhibition of transient receptor potential vanilloid-4 (TRPV4). Journal of Medicinal Chemistry, 62(20), 9270-9280.