Unveiling the Essentials: A Comprehensive Guide to Understanding and Managing Coronary Heart Disease and Angina Pectoris
Abstract
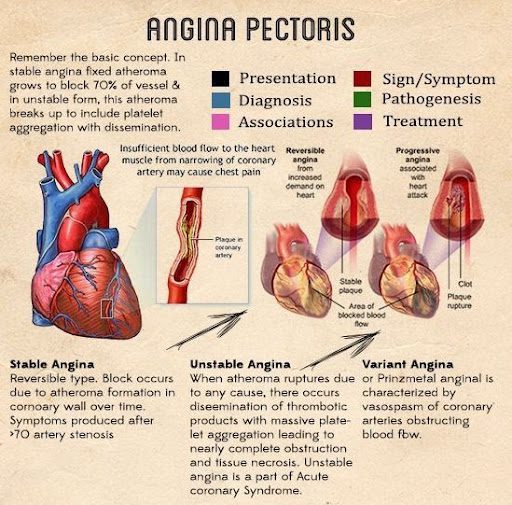
Coronary Heart Disease (CHD), also known as ischemic heart disease, is a leading cause of death globally. CHD is primarily caused by atherosclerotic plaque buildup in the coronary arteries, leading to restricted blood flow to the heart muscle. Angina pectoris, a common manifestation of CHD, is characterized by chest pain or discomfort resulting from myocardial ischemia-an insufficient supply of oxygen to the heart muscle compared to its demand.
Recent epidemiological studies highlight the increasing prevalence of CHD, attributing it to modern lifestyle factors such as poor diet, lack of exercise, and smoking. These factors contribute to the development of atherosclerosis, thereby increasing the risk of CHD. The early detection and management of these risk factors are critical in preventing the onset and progression of heart disease.
Angina serves as a critical warning sign for underlying coronary artery disease and often precedes more severe cardiovascular events such as myocardial infarction or sudden cardiac death. Understanding the symptoms and early intervention can significantly alter the disease course and improve patient outcomes.
In summary, CHD and angina pectoris remain significant public health challenges. The focus on early diagnosis, lifestyle modification, and therapeutic intervention is essential to manage and prevent these life-threatening conditions effectively.
Diagnosis and Symptoms of CHD and Angina
Diagnosing coronary heart disease (CHD) and angina pectoris relies heavily on recognizing the characteristic symptoms and employing diagnostic tests. The primary symptom, angina, manifests as chest discomfort or pain, typically provoked by physical exertion or stress and relieved by rest or nitroglycerin.
Diagnostic methods include non-invasive tests like electrocardiograms (ECG), which monitor the heart’s electrical activity, and stress tests that assess cardiovascular function under physical stress. Imaging techniques such as echocardiography and coronary angiography provide detailed views of heart structure and function, confirming the presence of blockages in coronary arteries.
Early and accurate diagnosis is crucial for effective management, guiding interventions that can alleviate symptoms and reduce the risk of more severe complications like myocardial infarction or heart failure. As such, healthcare providers emphasize the importance of regular screenings for at-risk individuals, which can lead to timely intervention and improved outcomes.
Non-Drug Treatments for CHD and Angina
Effective management of coronary heart disease (CHD) and angina pectoris significantly depends on non-drug interventions alongside traditional medical treatments. These interventions primarily focus on lifestyle modifications aimed at reducing the risk factors associated with heart disease.
Diet plays a pivotal role in managing heart health. A balanced diet low in saturated fats and cholesterol can significantly reduce plaque buildup in the coronary arteries, thereby improving heart function and reducing symptoms of angina. It is recommended to increase the intake of fruits, vegetables, whole grains, and lean proteins while limiting the consumption of red meats, processed foods, and high-fat dairy products.
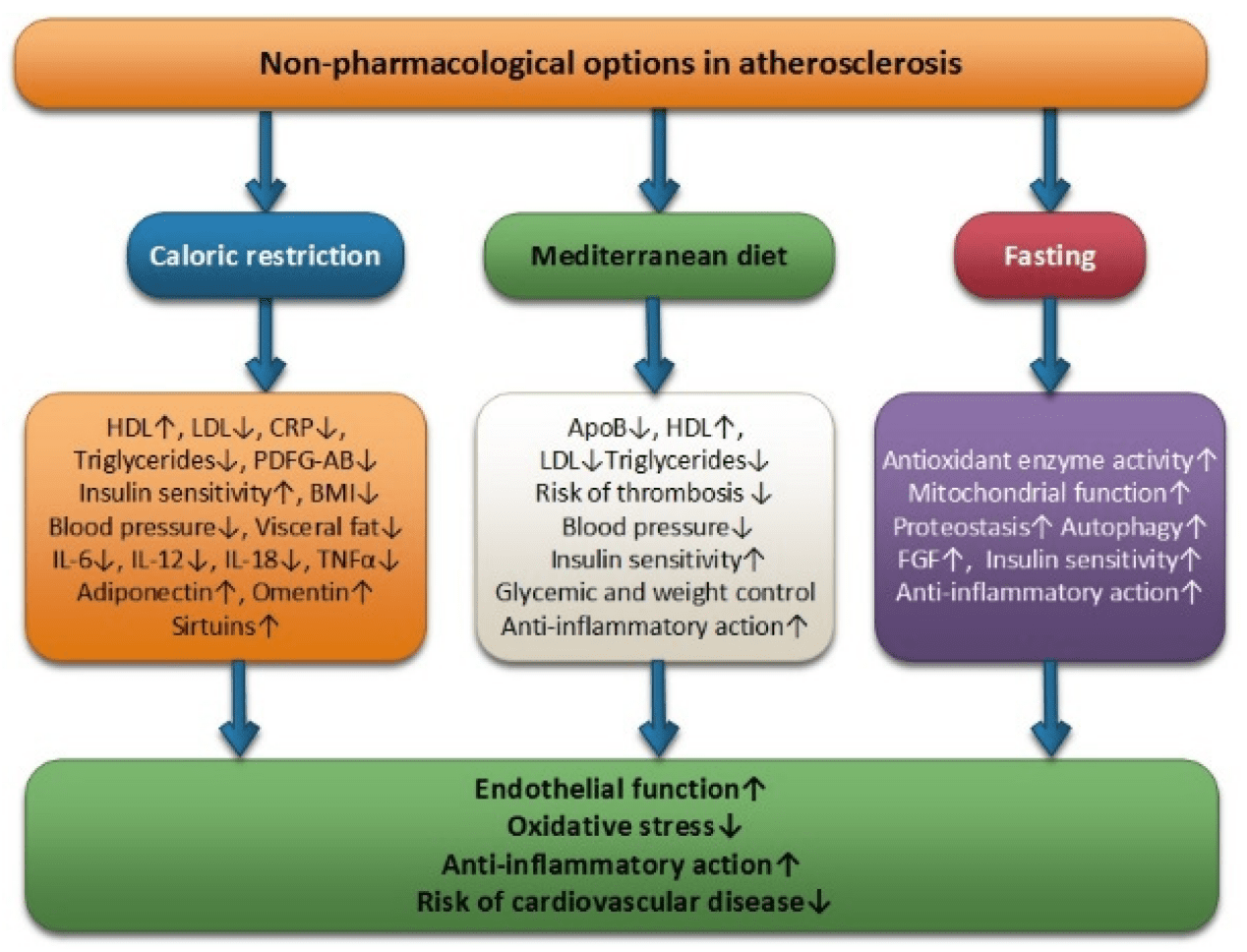
Physical activity is another cornerstone of non-drug treatment for CHD. Regular exercise helps strengthen the heart muscle, improves blood circulation, and helps control weight. It’s advised that individuals engage in at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous exercise each week. Activities could include walking, swimming, cycling, or other forms of cardiovascular training.
Smoking cessation is crucial as smoking directly contributes to the development of atherosclerosis and subsequently CHD. Quitting smoking can significantly improve cardiovascular health and reduce the risk of fatal heart events. Healthcare providers often recommend nicotine replacement therapies and counseling to aid in smoking cessation.
Stress management is also vital as stress can trigger angina attacks. Techniques such as mindfulness, yoga, and meditation can help manage stress levels. These practices not only improve psychological well-being but also have a positive impact on overall heart health.
Overall, these non-drug strategies are crucial for not only managing the symptoms of CHD and angina but also for improving life quality and longevity. They empower patients to take active control of their health and contribute to better clinical outcomes.
Pharmacological Treatments for CHD and Angina
Pharmacological management of coronary heart disease (CHD) and angina pectoris is essential for improving patient outcomes, managing symptoms, and preventing complications. The treatment strategy involves a variety of drug classes, each targeting different aspects of the disease pathology.
Nitrates, such as nitroglycerin and isosorbide mononitrate, are foundational in treating angina. They work by dilating blood vessels, which reduces the heart’s oxygen demand and relieves chest pain. Nitrates are effective for quick relief during angina attacks and for long-term management to decrease the frequency and severity of episodes.
Beta-blockers such as atenolol and metoprolol slow the heart rate and reduce blood pressure, lessening the heart’s workload. By decreasing the rate of heartbeat and the force of contraction, beta-blockers improve heart efficiency and reduce oxygen consumption, making them vital for chronic management of CHD.
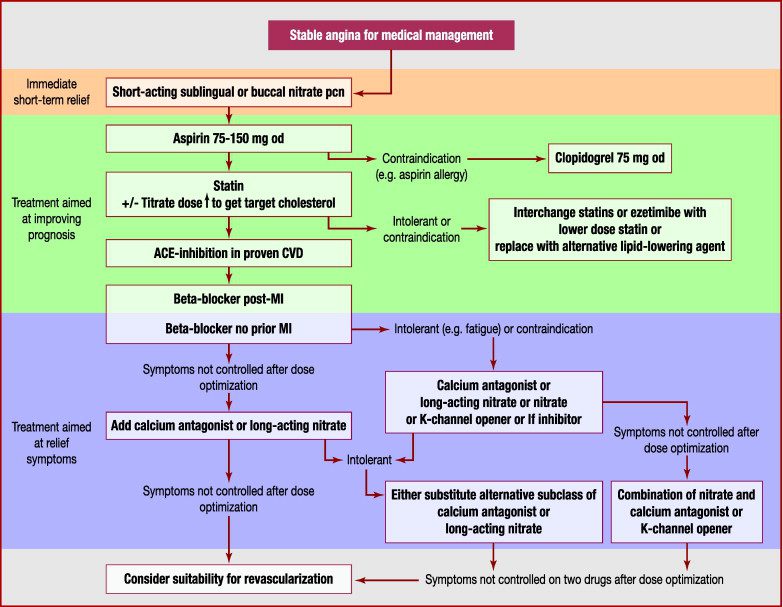
Calcium channel blockers like amlodipine and verapamil help in relaxing the coronary arteries and other blood vessels, further reducing the pressure and workload on the heart. These drugs are particularly useful in patients who cannot tolerate beta-blockers or have specific indications such as arrhythmias or hypertension coexisting with angina.
Antiplatelet agents, such as aspirin and clopidogrel, are prescribed to prevent platelet aggregation, reducing the risk of thrombus formation which can lead to heart attacks. Their use is recommended as a preventive measure in individuals with a high risk of cardiovascular events.
Statins are lipid-lowering medications crucial for managing cholesterol levels, a major factor in the progression of atherosclerosis. They are prescribed to virtually all patients with CHD, regardless of their initial cholesterol levels, due to their proven benefits in reducing cardiac events and mortality.
Each class of medications comes with its indications, dosage recommendations, and potential side effects, which must be carefully managed by healthcare providers. The choice of drugs and their combinations are tailored to individual patient profiles to optimize therapeutic outcomes and improve quality of life.
Long-Term Management and Prevention of CHD and Angina
Long-term management and prevention strategies for coronary heart disease (CHD) and angina pectoris are critical to reduce mortality and improve quality of life in patients. These strategies encompass both pharmacological treatments and lifestyle modifications, emphasizing continuity and adherence to prevent the progression of the disease.
Continuous Medication Regimen: For many patients with CHD, long-term use of medications such as statins, beta-blockers, and antiplatelet drugs is essential. These medications help manage cholesterol levels, reduce blood pressure, and prevent blood clot formation, which are crucial for preventing future cardiac events. Regular monitoring and adjustments by healthcare providers ensure that the medications continue to be effective and side effects are managed.
Lifestyle Modifications: Sustained lifestyle changes are equally important. Maintaining a healthy diet, engaging in regular physical activity, and avoiding tobacco products are foundational measures that help manage CHD. Patients are encouraged to adopt a heart-healthy diet rich in vegetables, fruits, whole grains, and lean proteins while limiting saturated fats and sugars.
Regular Screening and Monitoring: Regular check-ups and diagnostic tests such as blood pressure monitoring, cholesterol levels, and cardiac imaging studies help in early detection of potential problems and monitoring the effectiveness of the treatment plan. These screenings are vital for adjusting treatments as needed and for early intervention in case of new or worsening symptoms.
Patient Education and Support: Educating patients about the signs and symptoms of worsening heart disease and the importance of medication adherence is vital. Support groups and counseling can also play a significant role in helping patients adjust to lifestyle changes and cope with the chronic nature of their condition.
Integrated Care Approach: A collaborative approach involving cardiologists, primary care physicians, dietitians, and other health professionals is essential for comprehensive care. This team works together to tailor prevention and treatment strategies that best fit the individual needs of the patient.
References
- Komilovich, E. B. (2024). CORONARY HEART DISEASE. ANGINA TREATMENT. Journal of new century innovations, 46(1), 95-104.
- Axmedov, S. J. (2023). EFFECTS OF THE DRUG MILDRONATE. Innovative Development in Educational Activities, 2(20), 40-59.
- Gafurovna, A. N., Xalimovich, M. N., & Komilovich, E. B. Z. (2023). KLIMAKTERIK YOSHDAGI AYOLLARDA ARTERIAL GIPERTENZIYANING KECHISHI. ОБРАЗОВАНИЕ НАУКА И ИННОВАЦИОННЫЕ ИДЕИ В МИРЕ, 23(6), 26-31.
- Komilovich, E. B. Z. (2023). Coronary Artery Disease. EUROPEAN JOURNAL OF MODERN MEDICINE AND PRACTICE, 3(12), 81-87.
- Эргашов, Б. К. (2023). Артериальная Гипертония: Современный Взгляд На Проблему. Research Journal of Trauma and Disability Studies, 2(11), 250-261.
- Jamshidovich, A. S. (2023). THE ROLE OF THIOTRIAZOLINE IN THE ORGANISM. Ta’lim innovatsiyasi va integratsiyasi, 9(5), 152-155.
- Jamshidovich, A. S. (2024). NEUROPROTECTIVE EFFECT OF CITICOLINE. EUROPEAN JOURNAL OF MODERN MEDICINE AND PRACTICE, 4(1), 1-4.