Vorasidenib and Low-Grade Gliomas: A Promising New Therapy with Open Questions
Abstract
Low-grade gliomas (LGGs) are slow-growing yet malignant brain tumors that frequently harbor isocitrate dehydrogenase (IDH) mutations, which play a crucial role in tumor progression. Vorasidenib, a novel brain-penetrant IDH1/2 inhibitor, has emerged as a promising targeted therapy, offering an alternative to conventional treatments such as radiation and chemotherapy. The Phase-3 INDIGO study demonstrated that Vorasidenib significantly prolongs progression-free survival (PFS) and delays the need for additional therapies in patients with residual or recurrent IDH-mutant LGGs. However, several open questions remain regarding its long-term survival benefits, tumor response, and safety profile, particularly in comparison to standard multimodal treatment approaches. While Vorasidenib offers a non-invasive therapeutic option, further research is needed to determine its role in combination therapies and its potential to improve overall survival outcomes.
Introduction: The Need for Innovation in Low-Grade Glioma Treatment
Low-grade gliomas (LGG) are a group of slow-growing but malignant brain tumors that primarily affect young adults. Despite their relatively indolent nature compared to high-grade gliomas, these tumors can significantly impair cognitive function, neurological health, and overall quality of life. Over time, they have a high likelihood of progressing to more aggressive forms, such as glioblastoma, which drastically reduces survival rates. Consequently, there is an urgent need for innovative therapeutic strategies that can effectively manage tumor growth while preserving neurological function.
One of the most important breakthroughs in glioma research has been the identification of isocitrate dehydrogenase (IDH) mutations, which are present in approximately 70–80% of low-grade gliomas. These mutations lead to the production of an abnormal metabolite called 2-hydroxyglutarate (2-HG), which plays a key role in tumor development by altering the epigenetic landscape of cells. Given this unique metabolic vulnerability, researchers have been actively exploring IDH inhibitors as a targeted treatment approach.
Vorasidenib, a novel brain-penetrant IDH1/2 inhibitor, has recently emerged as a promising therapeutic candidate. Unlike other systemic IDH inhibitors, Vorasidenib is designed to cross the blood-brain barrier, making it particularly suited for treating gliomas. Preliminary studies have shown that Vorasidenib can reduce 2-HG levels in IDH-mutant tumors, potentially slowing disease progression and delaying the need for aggressive interventions such as chemotherapy or radiation.
The Phase-3 INDIGO study, recently published in the New England Journal of Medicine, has provided compelling evidence that Vorasidenib can significantly prolong progression-free survival (PFS) in patients with residual or recurrent IDH-mutant LGG. However, while the drug has demonstrated a clear benefit in delaying tumor progression, several open questions remain, particularly regarding long-term survival outcomes and potential resistance mechanisms.
In the following sections, we will explore how Vorasidenib works, key findings from the INDIGO trial, the limitations of the current research, and what the future holds for IDH-targeted therapies in glioma treatment.
How Vorasidenib Works: A Game-Changer for IDH-Mutant Gliomas?
Vorasidenib represents a novel approach to treating IDH-mutant low-grade gliomas (LGGs) by specifically targeting the metabolic vulnerability of these tumors. Traditional glioma treatments, such as surgical resection, radiation therapy, and chemotherapy, focus on either removing or destroying tumor cells. However, these methods often come with significant neurological side effects and may not prevent tumor recurrence. In contrast, Vorasidenib functions by directly inhibiting the mutated IDH1 and IDH2 enzymes, which play a crucial role in glioma progression.
In IDH-mutant gliomas, mutations in IDH1 or IDH2 lead to the abnormal production of 2-hydroxyglutarate (2-HG), a metabolite that disrupts normal cellular processes and promotes tumor growth. By inhibiting these mutant enzymes, Vorasidenib effectively reduces 2-HG levels, restoring normal metabolic function and slowing disease progression. This makes Vorasidenib a particularly attractive option for managing LGGs, as it offers a non-invasive, targeted approach that could delay or even reduce the need for aggressive treatments.
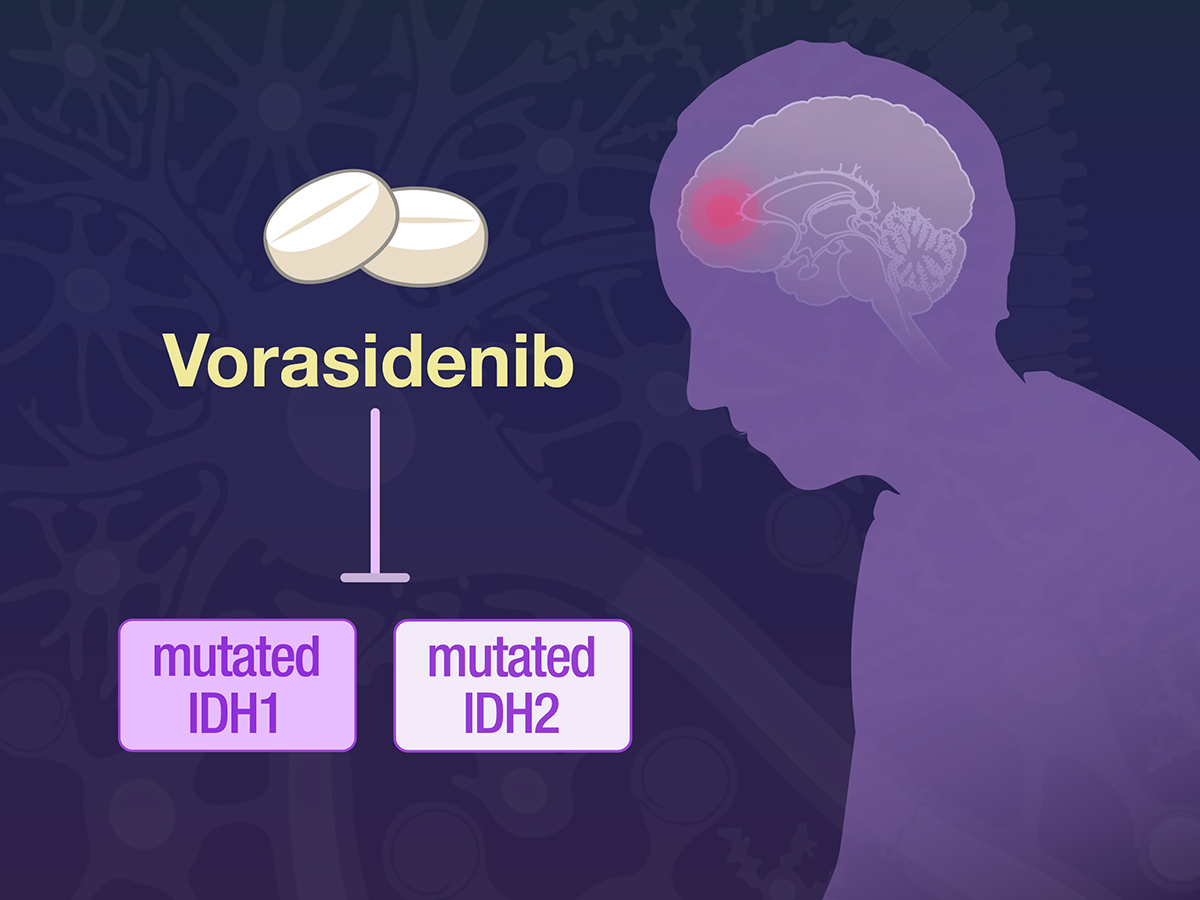
Fig 1. Vorasidenib in IDH-Mutant Glioma
A key advantage of Vorasidenib is its ability to cross the blood-brain barrier (BBB), which has historically been a major obstacle for many cancer therapies. Unlike other systemic IDH inhibitors, Vorasidenib is specifically designed to penetrate the central nervous system (CNS), ensuring that therapeutic concentrations of the drug reach the tumor site. This property significantly enhances its effectiveness in treating brain tumors compared to other IDH inhibitors, such as Ivosidenib, which has limited CNS penetration.
Clinical trials have demonstrated that Vorasidenib extends progression-free survival (PFS) in patients with IDH-mutant LGGs. By slowing tumor growth, the drug may allow patients to delay the need for radiation or chemotherapy, preserving cognitive function and quality of life. However, while Vorasidenib shows promise in controlling tumor progression, it is not yet clear whether it can induce tumor shrinkage or prevent the eventual transformation of LGGs into higher-grade malignancies.
As research continues, the future of IDH-targeted therapies may involve combination approaches, potentially using Vorasidenib alongside radiation or chemotherapy to achieve more durable and effective treatment outcomes.
Key Findings from the INDIGO Phase-3 Study
The Phase-3 INDIGO study represents a major milestone in the treatment of IDH-mutant low-grade gliomas (LGGs). Conducted as a randomized, double-blind, placebo-controlled trial, this study evaluated the efficacy and safety of Vorasidenib, a brain-penetrant IDH1/2 inhibitor, in patients with residual or recurrent LGGs. The goal was to determine whether this novel therapy could delay tumor progression and postpone the need for more aggressive interventions such as radiation or chemotherapy.
A total of 331 patients were enrolled in the study, with participants randomly assigned to receive either Vorasidenib (40 mg daily) or a placebo in 28-day cycles. The primary endpoint was progression-free survival (PFS), assessed via blinded MRI imaging by an independent review committee. An additional key secondary endpoint was the time until the next tumor-specific therapy was required.
The results of the INDIGO trial were highly promising. The median PFS in the Vorasidenib group was 27.7 months, compared to just 11.1 months in the placebo group. This represents a hazard ratio (HR) of 0.39 (p < 0.001), indicating a 61% reduction in the risk of disease progression or death. Additionally, the time to next intervention was significantly longer in the Vorasidenib group, with an HR of 0.26 (p < 0.001). These findings suggest that Vorasidenib has a clear ability to slow tumor progression and delay the need for additional treatments.
In terms of safety, Vorasidenib was generally well tolerated, but some notable side effects were reported. One of the most significant concerns was elevated alanine aminotransferase (ALAT) levels, a marker of liver toxicity, which occurred in 9.6% of patients receiving Vorasidenib, compared to 0% in the placebo group. Additionally, serious adverse events were more frequent in the Vorasidenib group (22.8%) compared to the placebo group (13.5%).
Overall, the INDIGO study provides strong evidence that Vorasidenib is an effective therapy for delaying tumor progression in IDH-mutant LGGs. However, further research is needed to determine its long-term survival benefits and its potential role in combination therapies.
Limitations and Open Questions About Vorasidenib
While the INDIGO Phase-3 trial has established Vorasidenib as a promising new treatment for IDH-mutant low-grade gliomas (LGGs), several limitations and unanswered questions remain. Despite its success in prolonging progression-free survival (PFS), the study raised concerns regarding long-term efficacy, tumor response, and safety.
One of the most critical limitations is that Vorasidenib does not significantly reduce tumor size in most patients. Unlike radiation and chemotherapy, which can shrink tumors, Vorasidenib primarily delays tumor progression rather than eliminating cancer cells. This raises concerns about whether the drug can truly alter the disease’s natural course or merely postpone inevitable progression. Notably, only 11% of patients in the INDIGO study showed measurable tumor shrinkage, indicating that the majority of tumors remained stable rather than regressing.
Another major concern is long-term survival outcomes. Although Vorasidenib extended PFS to 27.7 months, it remains unclear whether this translates into a longer overall survival (OS). In comparison, radiation combined with chemotherapy (PCV regimen) has been shown to provide a median OS of over 10 years in some patients. Given the INDIGO study’s relatively short follow-up period (14 months), more research is needed to determine whether Vorasidenib offers a meaningful survival benefit over traditional treatment approaches.
Additionally, there is limited data on how Vorasidenib interacts with other therapies. Since many LGG patients eventually require radiation or chemotherapy, understanding the effects of Vorasidenib as part of a multimodal treatment strategy is crucial. Questions remain regarding whether prior exposure to Vorasidenib could affect the efficacy of subsequent treatments, especially given that IDH-mutant gliomas have unique molecular and metabolic characteristics.
From a safety perspective, the risk of liver toxicity is another concern. The elevated alanine aminotransferase (ALAT) levels observed in 9.6% of patients receiving Vorasidenib suggest that regular liver function monitoring will be necessary for long-term treatment. Additionally, the long-term neurocognitive impact of prolonged IDH inhibition remains unknown.
Ultimately, while Vorasidenib represents an exciting advancement in glioma therapy, further research is needed to fully understand its role in clinical practice. Future studies should focus on long-term survival, combination therapies, and potential biomarkers to predict patient response.
Conclusion: The Future of IDH Inhibitors in Glioma Treatment
The development of Vorasidenib represents a significant step forward in glioma treatment, offering a non-invasive, targeted approach to managing IDH-mutant low-grade gliomas (LGGs). However, its long-term efficacy and optimal clinical application remain areas of active investigation.
The INDIGO Phase-3 trial has demonstrated that Vorasidenib prolongs progression-free survival (PFS) and delays the need for radiation or chemotherapy, which is especially valuable for younger patients looking to preserve cognitive function. However, whether this translates into longer overall survival (OS) remains unknown. Future research should focus on extended follow-up studies to clarify the long-term impact of IDH inhibition.
One potential avenue for improvement is the combination of Vorasidenib with other treatment modalities. While current data support its use as a monotherapy, integrating Vorasidenib with chemotherapy or radiation may enhance its effectiveness and provide more durable disease control. Additionally, ongoing research is needed to identify biomarkers that can help predict which patients will benefit most from IDH inhibition.
Another crucial consideration is patient selection. The INDIGO study focused on low-risk LGG patients, but it remains unclear whether Vorasidenib would be effective in higher-risk glioma patients or those with more aggressive tumor biology. Further clinical trials will be essential to determine the drug’s full therapeutic potential.
From a regulatory perspective, Vorasidenib is likely to be incorporated into clinical guidelines for IDH-mutant LGG management, particularly in patients who wish to delay radiation or chemotherapy. However, given the risk of liver toxicity and the need for long-term monitoring, careful patient selection and follow-up protocols will be critical.
In conclusion, Vorasidenib represents an exciting advancement in glioma treatment, but many unanswered questions remain. As additional clinical data emerge, the optimal role of IDH inhibitors in glioma management will become clearer, potentially leading to more personalized and effective treatment strategies for patients with IDH-mutant gliomas.
References
Baumert, B. G., Hegi, M. E., & van den Bent, M. J. (2016). Temozolomide chemotherapy versus radiotherapy in high-risk low-grade glioma (EORTC 22033-26033): A randomised, open-label, phase 3 intergroup study. The Lancet Oncology, 17(11), 30313-30318. https://doi.org/10.1016/S1470-2045
Mellinghoff, I. K., van den Bent, M. J., Blumenthal, D. T., et al. (2023). Vorasidenib in IDH1- or IDH2-mutant low-grade glioma. New England Journal of Medicine, 389(7), 589-601. https://doi.org/10.1056/NEJMoa2304194
Turcan, S., Rohle, D., Goenka, A., et al. (2012). IDH1 mutation is sufficient to establish the glioma hypermethylator phenotype. Nature, 483(7390), 479–483. https://doi.org/10.1038/nature10866
Douw, L., Klein, M., Fagel, S. S., et al. (2009). Cognitive and radiological effects of radiotherapy in patients with low-grade glioma: Long-term follow-up. The Lancet Neurology, 8(9), 70204-70202. https://doi.org/10.1016/S1474-4422
Mellinghoff, I. K., Penas-Prado, M., & Peters, K. B. (2021). Vorasidenib, a dual inhibitor of mutant IDH1/2, in recurrent or progressive glioma: Results of a first-in-human phase I trial. Clinical Cancer Research, 27(16), 4491–4499. https://doi.org/10.1158/1078-0432.CCR-21-0611
Mellinghoff, I. K., Lu, M., & Wen, P. Y. (2023). Vorasidenib and Ivosidenib in IDH1-mutant low-grade glioma: A randomized, perioperative phase 1 trial. Nature Medicine, 29(3), 615–622. https://doi.org/10.1038/s41591-022-02141-2
Pertz, M., Schlömer, S., & Seidel, C. (2023). Long-term neurocognitive function and quality of life after multimodal therapy in adult glioma patients: A prospective long-term follow-up. Oncology. https://doi.org/10.1007/s11060-023-04419-y